5 Reasons The NHS Is In Crisis Right Now

Nurses and supporters striking on a picket line outside St Thomas Hospital on the 20th of December 2022 in London, United Kingdom.
The NHS’s struggles are indisputable right now.
The historic backlog, the shocking A&E and ambulance waiting times, and the clear proof that NHS staff are stretched to breaking point – as some employees strike for the first time ever – all paint a pretty bleak picture for the health service’s future.
To make matters worse, the prime minister Rishi Sunak and the health secretary Steve Barclay are yet to propose an effective solution to the current crisis.
No.10 said on Tuesday that the government is “providing the NHS with the funding it needs”.
This came after concerns from the Royal College of Emergency Medicine warning that up to 500 people could die each week due to delays in emergency care.
Worries about the NHS’s collapse are nothing new and existed long before the pandemic – but the situation has come to a head following both Covid and Brexit.
Here are the main five reasons the health service is so stretched right now.
1. Demand
Population changes and an increase in patients with chronic or multiple conditions means there’s more demand for health services.
Not only did the pandemic add to the backlog by delaying treatment to most patients not struggling with Covid, but it has also left many with Long Covid.
This is on top of the worsening health of the UK population in general, a problem which started prior to the pandemic.
Simultaneously, we have fewer available beds and doctors per head than many comparable countries, according to the NHS Support Federation, resulting in rising waiting lists.
2. Spending
Pressure on the NHS has increased, in part because of years of austerity under successive Conservative governments.
The NHS has effectively been underfunded since 2010. Per head, the government spends less on the health service than many other comparable countries, the NHS Support Federation has claimed.
The government did pump more cash into it in both 2018 and 2019, but that still did not go far enough to plug the gaps.
The Financial Times has also claimed that “despite increases in day-to-day spending and staff numbers”, there still are not enough beds.
Without enough funding – and the correct management of such investment – frontline staff say they are not able to do their work properly, and that’s before they even get onto the topic of their own salaries.
The government has also asked for big efficiency savings which providers have found unachievable and driven up their deficits, according to the NHS Support Federation.
This all means that private sector companies are winning large contracts to run NHS services for profit.
3. Staff
As analyst Danielle Jefferies wrote in the British Medical Journal in June, “the workforce is the beating heart of the NHS but high vacancy rates mean it hasn’t got the capacity to keep pace with demand.”
Chronic work shortages mean more patients are left waiting.
It added: “Each delay caused by demand outstripping workforce capacity is having a knock-on effect somewhere else.”
On the surface it does look like there are more NHS staff, as the Institute for Fiscal Studies found in a report from December.
It said that the NHS has 12% more hospital doctors and ambulance staff and 8% more nurses now compared to before the pandemic.
But, it is treating 12% fewer patients from the waiting list than in 2019, and taking in 14% fewer emergency patients – showing it’s not just staff numbers, but deep-rooted issues causing the NHS collapse.
Dr Ian Higginson(Royal College of Emergency Medicine) - "We can't treat patients in corridors. We can't treat patients in car parks... our political leaders need to get out of their ivory towers to see what's going on on the front line.." pic.twitter.com/JS8AHbQRCn
— Haggis_UK 🇬🇧 🇪🇺 (@Haggis_UK) January 2, 2023
Nearly half of staff claim underfunding stops them doing their job properly, according to NHS Support Federation.
Then, there’s the problem with recruiting staff across the sector. With nurses striking for the first time, along with ambulance workers and other hospital workers, concerns over their pay and working conditions.
4. Capacity
Almost 14,000 beds are occupied by patients who no longer need to being hospital – that works out to be one in every seven.
Thousands of beds are then in effect unavailable for routine treatment, occupied by Covid patients or waiting to be discharged.
On top of that, much of the NHS is outdated, according to the FT’s John Burn-Murdoch. He claimed: “Record-keeping systems are so outdated that many English hospitals do not know how many staffed intensive care beds they have, making the planning of efficient transfer of patients in and out of beds a non-starter.”
Ambulances then get stuck waiting to hand over patients, leading to the closure of services.
The 18-minute safety standard for emergency ambulances hasn’t been met since July 2020, according to Jefferies’ article in the BMJ.
There are the growing number of people on the elective procedure waiting list to consider too – it reached 6.4 million in England back in June with one study from the University of Birmingham suggesting it would triple by 2030.
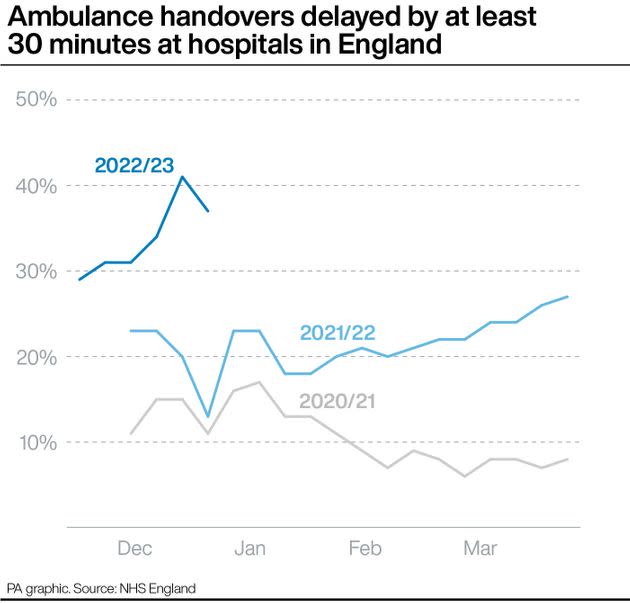
Ambulance handovers delayed by at least 30 minutes at hospitals in England
5. Social care
Large cuts to social care and mental health have added huge pressure, as it means patients who should be discharged from hospital and transferred to a social care facility are not able to.
As Jefferies alleged in the BMJ: “A combination of high vacancy rates in both health and social care is limiting the system’s ability to discharge patients into the community.”

 Yahoo News
Yahoo News 