How Bangladesh took on a global killer with the world's only diarrhoeal disease hospital

In Dhaka, Bangladesh, two-month-old Sammiya flops lifelessly in her mother’s arms, her eyes glazed over.
She is suffering from diarrhoea. This may not sound life-threatening – for most of us (in the West) diarrhoea is unpleasant, it might ruin a holiday or mean a few days off work at worst – but for many people across the world it is a killer.
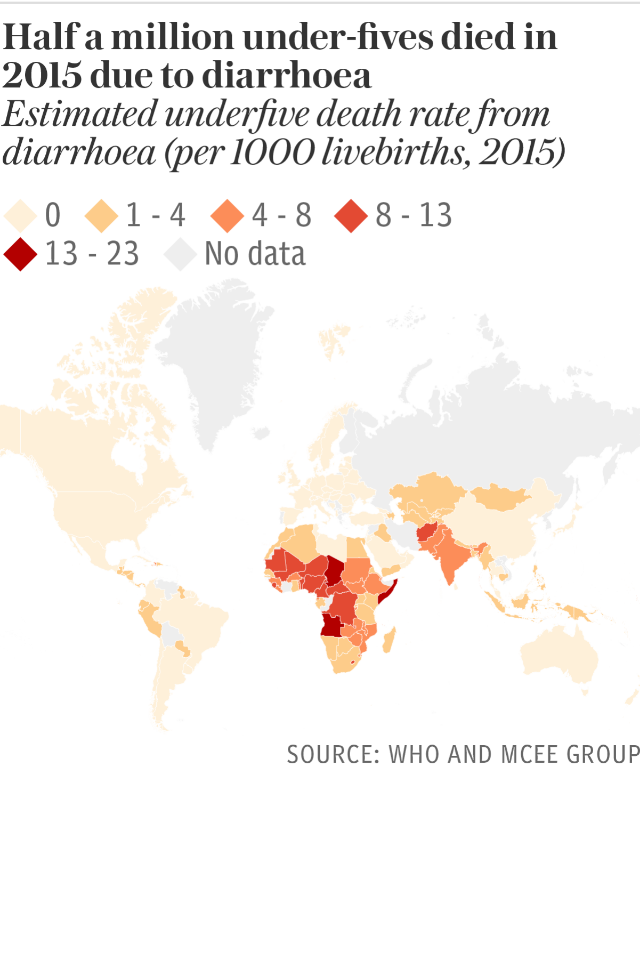
Globally, a child under five dies every two minutes as a result of diarrhoea: 500,000 a year. Sammiya will not be one of them. She is being treated in the International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR,B) in Dhaka, the only diarrhoeal hospital in world, which treats 220,000 patients a year.
As the birthplace of cholera – one of the biggest and deadliest causes of diarrhoea – Bangladesh has a lot of experience in dealing with diarrhoeal disease and, more recently, of doing so successfully.
Rather than a disease itself, diarrhoea is the symptom of an infection. In the ICDDR,B clinic in Dhaka, for example, around 20 per cent of the patients come in suffering from cholera, and the rest from rotavirus, shigella, salmonella and e-coli.

Globally, rotavirus is the most common cause of diarrhoea. Understanding how such diseases are spread long baffled doctors. In the 1800s when epidemics of cholera started to break out around the Bay of Bengal they were blamed on ‘miasma’: noxious particles in the air.
Only in the 1880s did scientists discover that the bacteria which causes cholera is waterborne – thriving in salty water. “It then took a hundred years, until the 1980s, for them to find out why – because it lives in algae,” says Dr Sirajul Islam, explaining how cholera epidemics occur twice a year: when the algae bloom in the pre- and post-monsoon seasons.
From the swampy water the cholera bacteria finds it ways into human’s systems through consumption. It is then passed along in what is known as the faecal oral route: human faeces (containing the bacteria) contaminates water which is then consumed by another person.
Most of the diarrohea-causing infections are spread this way. In rich countries faecal contamination is rare, but in the developing world surprisingly, or perhaps unsurprisingly, it is common. With nastier bugs causing diarrhoea, deaths are also more frequent.
Cholera is not like other diarorheal diseases, you can lose 50 per cent of your body weight in hours: people often arrive here with barely traceable pulses
Dr Firdausi Qadri
“Cholera is not like other diarrhoeal diseases,” says Dr Firdausi Qadri “you can lose 50 per cent of your body weight in a very short space of time, hours: people often arrive here with barely traceable pulses.”
Less than 50 years ago whole villages would be wiped out by cholera epidemics. The other factors that make diarrhoea deadlier in developing countries are access to adequate healthcare, the individual’s immunity and general health.
In countries where malnutrition effects large swathes of the population, for example, and where people live in overcrowded dirty conditions, immune systems are weaker, particularly among children.
Death from diarrhoea, as such, becomes a real risk. Since 2005, however, the global mortality rate among children under five, as a result of diarrhoea, has dropped by 40 per cent, and overall by around 20 per cent. Some regions have seen bigger reductions, for example south east Asia saw a 65 per cent reduction. Bangladesh leads the pack, though.
According to statistics from the World Health Organization (WHO), in 2003, diarrhoea killed more than 560 per million in Bangladesh. By 2013 this had been reduced to 145, and last year to three: a 95 per cent reduction. A wander around the ICDDR,B hospital in Dhaka explains some of this success.
Patients, divided into three wards depending on the severity of their illness, lie in neat rows of cholera cots – hospital beds with holes in the centre and buckets beneath – which allow nurses and doctors to accurately assess how much water they have lost and replace it.

The sicker patients are hooked up to saline fluids, while others are spooned oral rehydration solution by nurses and relatives.
“You’ll notice it doesn’t smell,” says Dr Azharul Islam Khan, “cleanliness is very important.” The only odour is antiseptic. Aside from those with complications, everyone is discharged with 36 hours.
The system is a slick, well-oiled machine. The upper floors of the ICDDR,B building are home to some of the country’s other secret weapons: its scientists.
In the 1960s ICDDR,B scientists invented the oral the rehydration solution (ORS), which the WHO estimates, since then, has saved millions of lives. Thirty years later researchers found that zinc treatment shortened the duration of diarrhoea and prevented future cases, particularly in children – a discovery responsible for the reduction of infant deaths world over.
Most importantly, these innovations are dirt cheap and, as such, have been easily up-scaled across the country.
“Every single house in the rural in Bangladesh can make their own oral rehydration solution at home – even the very poorest,” Dr. Hammam El Sakka, team leader for Emergency Health Response, WHO Bangladesh.
The government’s strong network of community healthcare workers and volunteers have also been crucial in this. They quickly identify and treat cases of diarrhoea at a community level, and refer those in need of more intensive treatment on to local clinics.

This structure also means it is easy spot early warning signs of clusters and implement a fast response to avoid epidemics. Still, prevention is better than cure. Here, the challenge remains.
“Because of the increased capacity to treat diarrhoea, which means fewer people are dying now,” says Dr Khairul Islam, from WaterAid, Bangladesh. “It doesn’t get much attention on a government level anymore.”
The same seems to be true, and perhaps more so, elsewhere: while the global mortality rate has dropped significantly, the number of cases has only fallen by 10 per cent in the same period, and in many countries not at all.
Even when not fatal, the impact of diarrhoea should trouble governments. In countries where people can only dream of such a luxury as sick pay, parents taking a few days off work to look after an ill child can easily push their whole family back into poverty – or prevent them getting out of it.
On a larger scale, this ‘health shock’ phenomenon has an impact on struggling economies. For children, diarrhoea, in particular, also often leads to or is associated with other secondary diseases and conditions, like pneumonia, malnutrition and stunting.
The latter two have a knock-on impact on long-term health and a child’s development and, studies show, their future productivity – again, when considered on a large scale, hindering nascent economies. One preventative measure is vaccination.
An oral cholera vaccine has been available since the early 1990s and a rotavirus one from around ten years ago. ICDDR,B has carried out large vaccination studies throughout Dhaka’s slums and parts of rural Bangladesh – and more recently in the Rohingya refugee camps.
From last November, partner organisations implemented the vaccinations, giving some 900,000 doses of cholera vaccine to refugees. And a new round of vaccinations began on May 6.
Until recently, the oral cholera vaccine was believed require two doses, spread at least several weeks apart. The recent studies, however, show that for people over the age of five, whose immune systems are more developed, one dose is sufficient – and more practical, particularly, in crisis situations.
In such a situation, the vaccination programs make a great deal of difference, says Dr Qadri – noticeably there has been no cholera outbreak in the camps, despite the dire sanitary conditions – but “vaccination is a only short-term solution: a stop gap.”
The cholera vaccine, in low-income settings, is about 50 to 60 per cent effective. WaterAid has similarly found that the rotavirus vaccine has an efficacy rate of just 46 per cent.
Hand-washing alone (after going to the toilet and before eating), however, reduces diarrhoea by up to 48 per cent. In the long-term, any solution needs to include improved access to clean water, sanitation facilities and hygiene practices.

Across the world, one in nine still live without access to safe water, and each day, 2.3 billion people defecate outside, while only 19 per cent of people wash their hands.
Bangladesh has made a start in these areas. Just over ten years ago “half of the country was taken over by NGOs,” says Dr Khairul Islam. These NGOs – particularly the Bangladeshi mega-charity BRAC – alongside the government, went on a mission to build latrines across rural parts of the country.
Working in a very coordinated fashion, they were very successful. Between 2006 and 2015 five million households built latrines. India is currently on a similar campaign to build toilets.
“There is a huge political commitment to reach every part of the country,” says Arundati Muralidharan, policy manager for WaterAid, India. “But it is an enormous country, far larger than Bangladesh, with lots of remote pockets.”
Regardless of the number of latrines being built, the fact remains: rural Bangladeshis use them, rural Indians less so. The numbers are contested but, according to the WHO, around 40 per cent of people still openly defecate in India, and less than 1 per cent in Bangladesh.

One key difference may be the environment. Bangladesh has a population of 170 million in an area only twice the size of Ireland: as forests are torn down to make way for people, even in rural areas there are fewer outdoor places people can find privacy.
This is less the case in rural India. According to Dr El Sakka and Dr Khairul Islam, though, the main reason open defecation has been eliminated in Bangladesh is through attitude change. Today, having a latrine is seen as a mark of respectability.
“The community-led sanitation programme in the 2000s created a huge social movement across the country in favour of latrines,” says Dr Khairul Islam. “It was started by NGOs but people carried it on themselves.”
Cash incentives to keep girls in schools during this time, particularly in rural areas, played a a role too, according to Dr Khairul Islam.
Girls put pressure on their parents to use the extra money to build a latrine. In fact, he suggests, women are at the centre of the “name and shame game” which has so effectively changed Bangladeshis’ toilet habits.
Educating people is not enough to change behaviour. You have to motivate them
Dr Om Prasad Gautam, WaterAid UK
The most effective way to encourage the building and use of latrines, he says, is to ask men: “Where will your woman go? It is a matter of shame and disgrace that you can’t protect your daughter, your wife, your sister, you’re allowing them to be exposed in front of others.”
Today, when describing why she uses a latrine Salma, who lives in Dighaldi, a small village near the town of Matlab, does not mention hygiene or the risk of diarrhoea.
“It would be a great shame on my family for me to 'go’ outside,” she says. “If someone goes in the open children will be blowing whistles.”
“The trick is to change social norms,” says Dr Om Prasad Gautam, public health expert, and behaviour change scientist at WaterAid UK. “Educating people is not enough to change behaviour. You have to motivate them.”
Dr Gautum recently led a pilot project in Nepal based on this theory.

Working with the ministry of health – which is in the process of introducing a rotavirus vaccine – they enlisted 2,200 female community volunteers in four districts, to target five key behaviours during the vaccination campaign: exclusive breastfeeding up to six months, food hygiene, hand-washing, water treatment, and latrine-use (including for small children).
“First you need to understand what will motivate people,” says Dr Gautam.
In Bangladesh notions of shame around women exposing themselves has helped push a cultural shift away from open defecation. In Nepal, similarly they found that while telling people hand-washing will kill bacteria has little effect – “people cannot see bacteria,” emphasises Dr Gautam – telling people hand-washing gets rid of dust and dirt, and will make their hands look nicer and make them more respectable makes a real difference.
Similarly, telling mothers heating the food will make it tastier and their children will eat more is more effective than lecturing them on reducing bacteria.

It seems people respond particularly well to public praise. Dr Gautam and his team promoted the notion of an ideal family, telling mothers: “If you want to be an ideal family, first get your children vaccinated and then practice these five things.”
Those who achieved this were then publicly rewarded with branded mirrors, for example, which they could display in their houses.
Before the project, only 5 per cent of mothers in the four districts were practicing all five of the key behaviours. By the end of the project, this had risen to 53 per cent.
Although, the direct impact on the rate of diarrhoeal disease has yet to be assessed, “results look promising” according to Dr Gautum, who is in talks with other governments, such as Uganda, about introducing elements of this package during other vaccination programmes.
In Bangladesh, ICDDR,B, and other organisations such BRAC, are beginning integrated approaches, combining vaccination and behaviour-changing strategies.

Open defecation may be a thing of the past, but other obstacles remain. Dr Sirajul Islam, for example, has found even where ground water is clean, the mouth of tube wells where people access it are often rimmed with dirt, and the water people have in their homes, stored in open buckets, is teeming with bacteria.
As such, he has created a cheap formula to purify water and kill cholera-causing algae: the Siraj Mixer. But as with chlorination and boiling, many Bangladeshi still do not think to treat water before consuming it. Nor do they heat food properly or wash their hands.
“We still need to find ways of getting people to do these things,” says Dr Sirajul Islam.
Dr Gautam agrees. “Across the global south, there is a long way to go, but we’re getting there,” he says.
Hopefully, when they do, they will share their answers with the developed world.
People in countries like the UK may not die from diarrhoea, but only 44 per cent of Britons wash their hands after going to the toilet – we still have a thing or two to learn about hygiene.

Protect yourself and your family by learning more about Global Health Security

 Yahoo News
Yahoo News 