Chronic pain sufferers should not be given opioids, says medicines watchdog
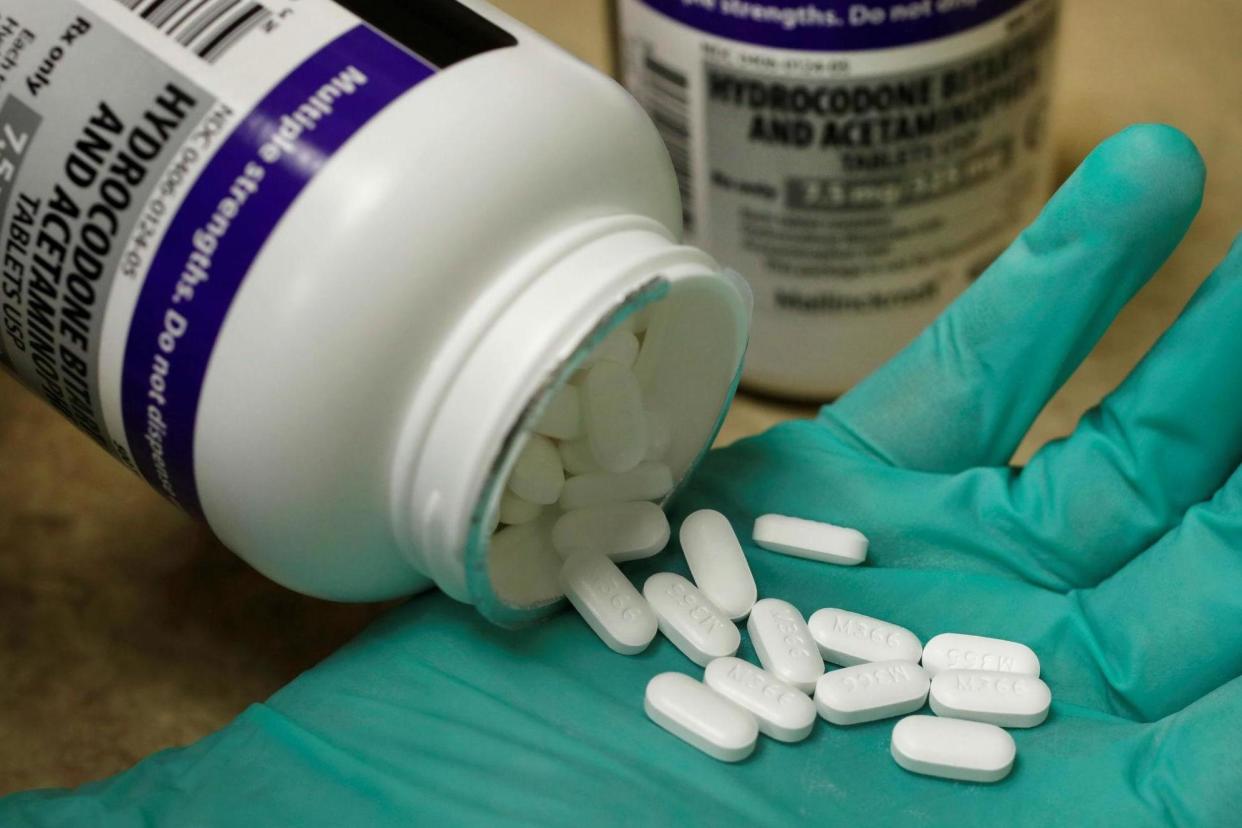
People with chronic pain that can’t be explained by other conditions should not be prescribed opioids because they do more harm than good, the medicines watchdog has warned.
The National Institute for Health and Care Excellence (NICE) has said people should instead be offered group exercise, acupuncture and psychological therapy.
In new draft guidance, NICE said most of the common medications used for chronic primary pain has little or no evidence to support their use in patients aged over 16.
Its latest guidance comes amid concerns over the level of opioid use. In September last year a review by Public Health England found 1 in 4 adults have been prescribed addictive medications with half of them taking the drugs for longer than 12 months.
Between 2017 and 2018 this meant 11.5 million adults in England received a prescription for an addictive medication such as opioids.
NICE’s new draft guidance said some antidepressants should be considered for people with chronic primary pain but it said paracetamol, non-steroidal anti-inflammatory drugs such as aspirin and ibuprofen, as well as benzodiazepines or opioids should not be given because of concerns they might do more harm than good.
Chronic primary pain is a condition in itself and is not a symptom of another condition. It is often linked to emotional distress and functional disability. NICE said examples include chronic widespread pain and chronic musculoskeletal pain, as well as conditions such as chronic pelvic pain.
Chronic pain may affect between a third and one-half of the population. Almost half of people with chronic pain have a diagnosis of depression and two-thirds of those suffering are unable to work because of it.
Nick Kosky, a consultant psychiatrist at Dorset HealthCare University Foundation Trust and chair of the guideline committee said: “Understandably, people with chronic pain expect a clear diagnosis and effective treatment. But its complexity and the fact GPs and specialists alike find chronic pain very challenging to manage, means this is often not possible.
“This mismatch between patient expectations and treatment outcomes can affect the relationship between healthcare professionals and patients, a possible consequence of which is the prescribing of ineffective but harmful drugs.
“This guideline, by fostering a clearer understanding of the evidence for the effectiveness of chronic pain treatments, will help to improve the confidence of healthcare professionals in their conversations with patients. In doing so it will help them better manage both their own and their patient’s expectations.”
Paul Chrisp, director of the centre for guidelines at NICE, said: “What this draft guideline highlights is the fundamental importance of good communication to the experience of care for people with chronic pain.
“When many treatments are ineffective or not well tolerated, it is important to get an understanding of how pain is affecting a person’s life and those around them because knowing what is important to the person is the first step in developing an effective care plan.
“Importantly the draft guideline also acknowledges the need for further research across the range of possible treatment options, reflecting both the lack of evidence in this area and the need to provide further choice for people with the condition.”
A consultation on the proposed new guidelines will run until Monday 14 September 2020.
Read more
Time to run the NHS at the top of its game, not top of its capacity
Scandal-hit NHS trust admits to negligence in death of six-week-old
Government scraps quarantine exemption for NHS and care workers

 Yahoo News
Yahoo News 