When Will There Be A Coronavirus Vaccine?

In the mid-2010s, an outbreak of Ebola ravaged West Africa. Between December 2013 and June 2016, the disease officially killed 11,308 people in Liberia, Guinea and Sierra Leone, although the World Health Organisation (WHO) believes the real figure is probably much higher.
Ebola's virulence and lethality – it has a mortality rate of around 40 per cent; Covid-19, the disease caused by the novel coronavirus, kills roughly one per cent of sufferers, although the exact number is currently unclear – made containing it an international priority. By mobilising labs around the world, a prophylactic Ebola vaccine – rVSV-ZEBOV – was rushed through development. In December last year, six years after the first cases were discovered in West Africa, and three years after the outbreak was officially deemed over, the Food and Drug Administration (FDA) finally OKed it for use in the US. Compared to the normal timelines for these things, that still represents astonishing speed.
In the wake of the Ebola outbreak, WHO has taken a front-foot approach. Every year it publishes a list of key diseases it sees as the major issues the medical research community needs to tackle. The Blueprint For Diseases, as it’s called, highlights the diseases that could break out into epidemics in the next 12 months. It's a guide for the research community, an attempt to steer its resources to where they're most required. Currently, Covid-19 tops the list. Lurking at the bottom, as it has been every year since the Blueprint was first published in 2016, is something that sounds like it's been pulled from the pages of a comic: Disease X.
“That’s the unknown, brand new pathogen that springs up,” says Rachel Grant, of the Coalition for Epidemic Preparedness Innovations. CEPI was formed in 2017, after the Ebola crisis made apparent the lack of a single, coordinating voice in the research and development (R&D) of vaccines. Its founding partners included the nation of Norway, the Gates Foundation, the Wellcome Trust, and the UK Research Foundation. (Since then, Germany and Japan have signed up, too.) “What happened with Ebola was the world tragically realised they reacted too late," says Grant. "The whole system was too fragmented to respond in an effective way.”
Disease X has long been recognised as an issue. Before coronavirus, the last brand new pathogen to spring up was the mosquito-borne Zika virus, which infected an estimated half-a-million people between 2015 and 2016. At the time of writing, Covid-19 had infected at least 1.5 million people and killed 90,000 (see the most recent numbers at Johns Hopkins University’s live map of global cases).
The worldwide count of confirmed #COVID19 cases, according to John Hopkins University, has exceeded 1.5 million. (The number of actual cases, not confirmed by testing, will be much larger.)https://t.co/ipIrDfNylG pic.twitter.com/6FnaKE7yv5
— Peter Aldhous (@paldhous) April 9, 2020
The focus of the R&D world is now squarely on Covid-19, and the race is on to develop a vaccine. If the boffins and academics are to succeed, they will have to move at a previously unheard-of pace. Vaccine researchers are used to working on vaccines for decades, but with coronavirus, we can’t wait that long. More than 60 teams across the globe are trying to find a way to protect the world’s population – up from around 40 two weeks ago – and the more optimistic among them think there could be a vaccine ready in 12 to 18 months. “That is unprecedented in human history,” says Grant. “No vaccine has ever been developed at that speed.” But they have to try.
Professor Katie Ewer hated immunology when she was an undergraduate. She had been interested in biology since she was a child, fascinated by seemingly endless processes that occur in our cells and organs every second of our lives without us knowing about it. When she didn't get into medical school she trained as a microbiologist instead, and grew fascinated by infectious diseases. “I’ve always had a real obsession with the human body, anatomy and how it works,” she says. Eventually, she came to see immunology as its "ultimate expression". After a PhD in the subject she landed at Oxford University's Jenner Institute, and has spent the 13 years since working on a malaria vaccine, to try and halt the spread of a disease that kills 500,000 people every year.

Thirteen years may sound like a long time, but vaccines are difficult to develop, especially when they're for diseases that largely impact the poorer parts of the world. A malaria vaccine would save tens of millions of lives, but it would be less profitable than, say, a drug that reverses hair loss or makes you lose weight. So not-for-profits like the Jenner Institute, where Ewer is a senior scientist, do the work that big pharma won't prioritise. According to The Global Fund, $5 billion is needed to keep development of a malaria vaccine on track. In 2018, researchers received $2.8 billion, a drop from the year before. That Covid-19 has spread through the global west has, perversely, probably accelerated the search for its vaccine.
To create a vaccine, you need to know what you're fighting, which is why, on 11 January, researchers in Shanghai leaked the genetic sequence of the coronavirus, after realising that Chinese authorities had no intention of releasing it globally. The next day, their lab was closed for "rectification". Their sacrifice enabled teams around the world to mobilise.
Vaccines work by training your body to react in a certain way, like teaching a child to catch a ball. The first time you throw it, it bounces off them. The second time, maybe they put up an arm to protect themselves. Eventually, they'll learn to predict its flight, get their hands in the right place, and time when they should wrap their fingers around the ball. It's become an innate reaction that happens almost without thinking.
In the same way, the first time your body is exposed to a new virus, it doesn't know how to react. Being infected with Covid-19 is like turning a tennis ball launcher on that child before they've learnt to catch – they'll be overwhelmed. But introduce a measured, non-fatal dose and our body learns to battle it, even when confronted by a larger amount. This is done by injecting antigens (or small molecules of the virus, which is a pathogen) into the body. The immune system recognises a harmful alien presence and, through a process of trial and error, creates antibodies to battle it. Once it's been destroyed, your body remembers the specific antibodies it needs to produce if the virus returns – say, through live infection – so it can mobilise more quickly. (This is also why those who've already been infected almost certainly can't catch Covid-19 a second time, unless the virus mutates.)
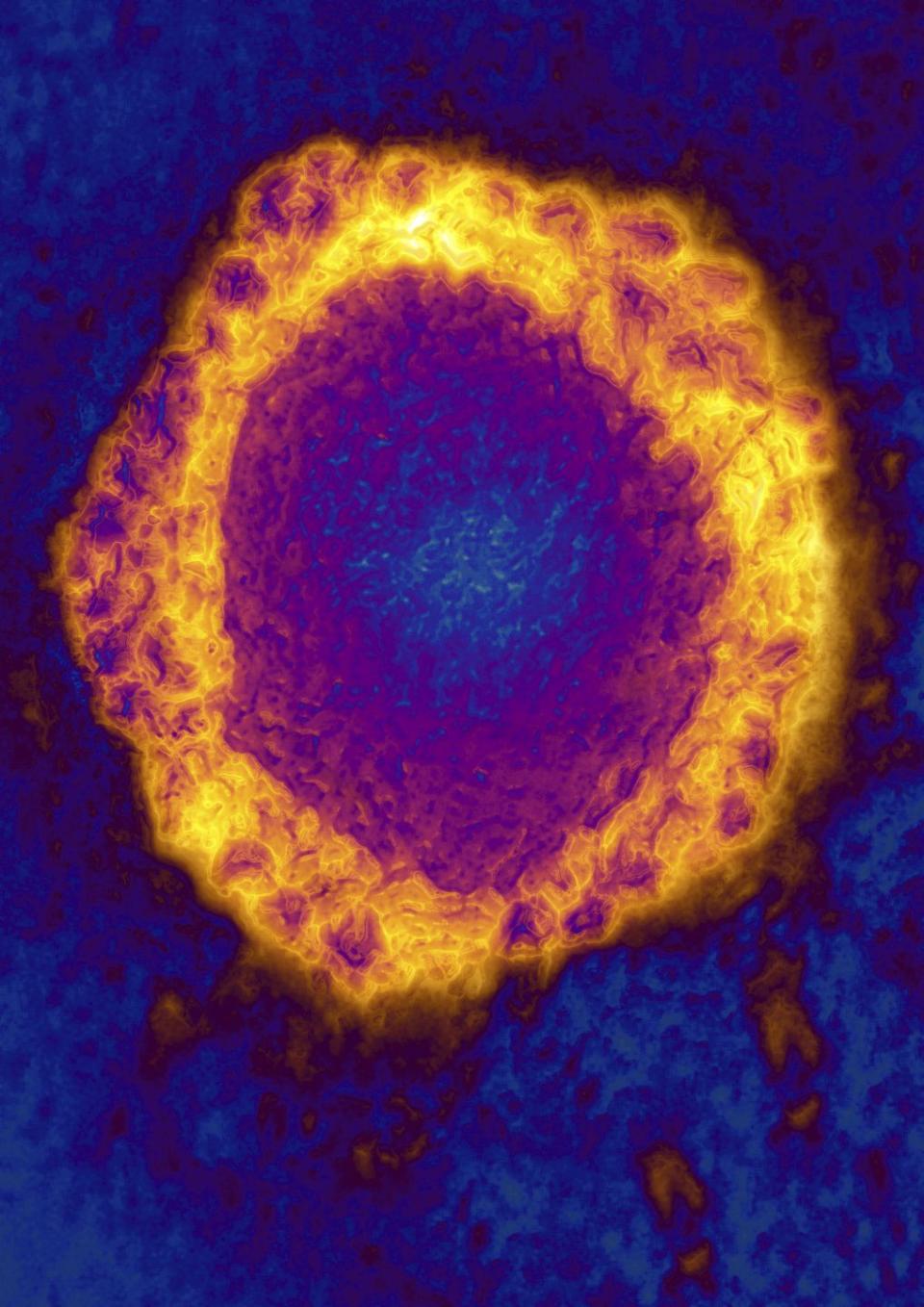
Before the advent of genetic medicine, vaccines worked by injecting patients with either a dead form of a virus, so it couldn't replicate inside the body, or a similar but less harmful pathogen (Edward Jenner, for whom the Jenner Institute is named, all-but invented vaccination in the 1790s when he realised that if you deliberately infected someone with the comparatively harmless cowpox virus, they wouldn't catch smallpox). Today, making a vaccine isn't simple, but it is standardised. “The actual platform – the backbone of the vaccine – is always the same, whatever the disease,” says Ewer. Researchers just slot in a little bit of the genetic information from the new virus.
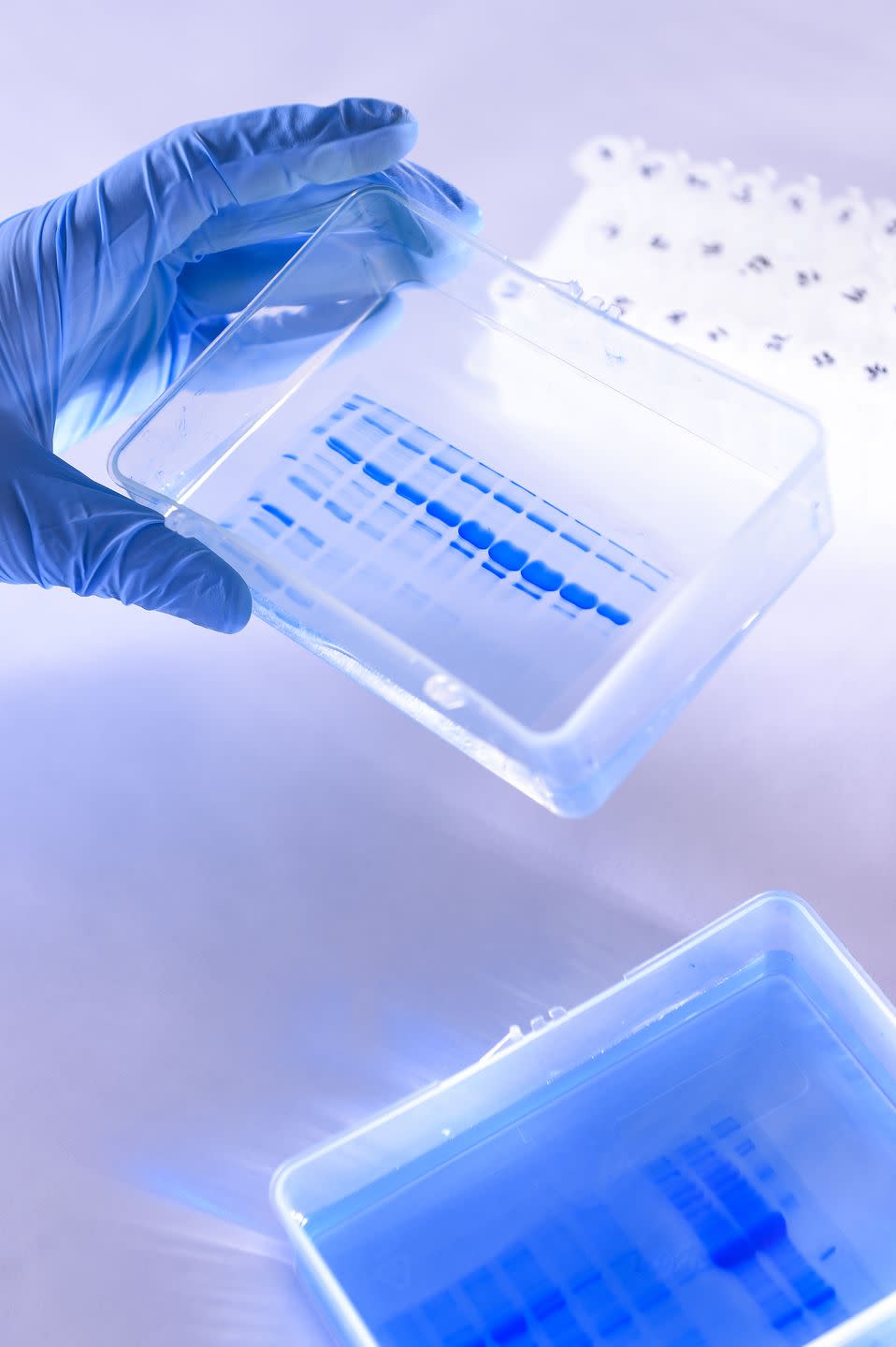
The Jenner Institute develops a multitude of different vaccines at any one time, and at the start of the year, Ewer’s colleague, Professor Theresa Lamb, was handling its coronavirus research. By the middle of February, the Institute had recognised that the early stages of their vaccine production had gone well, and were preparing to test it in a clinical trial. Suddenly the small number of people working on the vaccine under Lamb ballooned. Ewer was drafted to help in the effort, one of around 60 people – including doctors and nurses who are screening potential trial participants and laboratory staff developing tests and assays – working on the project. Many are working from home: the lab doesn’t want people in unnecessarily, in case they contract or spread the disease. “We go round [the laboratory] with a tape measure, we measure two metres, work out the number of people who can safely work at that distance in a particular area of the lab,” says Ewer. “It’s really boring, just the same as any other supermarket or shop.”
The potential outcome is far from boring. “Covid-19 has changed our scientific landscape in terms of how fast things are moving,” says Dr Melvin Sanicas, a vaccinologist and medical director at Takeda, a Japanese pharmaceutical company. Since its genetic sequence was released, two teams have got candidate vaccines into clinical trials. One is based on an Ebola vaccine, developed by CanSino Biological Inc, a Hong Kong company, in collaboration with the Beijing Institute of Biotechnology. The other is from a Massachusetts-based pharmaceutical company, Moderna (who declined to speak for this story).

In the 70 years since the first identified coronavirus infection in humans, no vaccine has ever got beyond Phase II trials, which means labs are taking diverse approaches to finding one now. The Asian plan uses a non-replicating viral vector – essentially, the dead vaccine. The Moderna plan uses an RNA vaccine, in which human cells are injected with the disease's RNA – a simpler version of DNA, used by cellular organisms like viruses – in the hope that it will absorb it and start to produce antibodies. The former isn't so different from Jenner's original method; the Moderna plan is based on science that, so far, is largely theoretical, but which will be much quicker to test and produce than those made by the traditional method. If it works.
But finding a vaccine that defeats a disease is merely step one. “You test the vaccine candidates in cell cultures or animal models to see if the vaccine candidate is safe and whether it’s able to induce an immune response,” says Sanicas. The right immune response sees the body fight back against the pathogen, without being overwhelmed by it – some candidate vaccines have to be shelved because the virus wins. Get it to work in cell cultures or animal models, and you’re through the pre-clinical phase. You can now try and test it in humans.
Testing is the time-consuming part. The team at Oxford University recently put out a call for participants across the Thames Valley area, asking for 510 participants in total. More than half will be given the actual vaccine, and 250 will be given a control. They’ll be monitored over the next six months to see how the vaccine is working – researchers are looking for an immune response, but also check for side-effects that might be worse than the disease. In exchange, the participants will get up to £625, and the pride of knowing they’re helping save the world. The amount is relatively low (participants in a botched clinical trial in the mid-2000s got £2,000 each), and the risk real: an accompanying document acknowledges “with any vaccination there is a risk of rare serious adverse events”.
All vaccines entering clinical trials on humans go through three stepped stages. The Oxford trial will test only a few people to start with, to make sure everything works correctly and safely, before increasing the numbers. “We’ll try and get up to vaccinating some quite big numbers of people in a short space of time,” says Ewer. In less urgent times, that means thousands of participants over several years, because it can take months for an immune response to show up in healthy subjects.
To progress, a vaccine needs to produce positive results at all three stages. Normally, that means an effectiveness of at least 97 per cent, says Sanicas, although the pandemic is so severe that any potential coronavirus vaccine could be rolled out with results as low as 70 per cent.
Next, you start applying to national regulatory bodies – the FDA in the US, the Medicines and Healthcare Products Regulatory Agency in the UK, and the European Medicines Agency in the EU – for approval. “Once they’ve determined the vaccine is safe, effective and made using quality production mechanisms, they approve the vaccine for use,” says Sanicas. Getting from identification to commercial vaccine normally takes the best part of a decade.
Faced with a pandemic, there's always a temptation to cut corners. Every extra day jumping through red tape means thousands of people dead, tens of thousands more infected. But the scientific community has learned that a bad vaccine is worse than no vaccine. In the mid-2000s, trials of an experimental leukaemia drug in London went wrong, seriously damaging six participants – without that testing, actual patients could have been given a drug that was more likely to kill them than their disease. And all vaccine development lives in the shadow of a terrible series of events in 1976, when the threat of a swine flu epidemic across the US led the government to instigate mass vaccination. To speed up production, they opted to use a "live" virus, rather than an inactive strain. Of the inoculated, one in 100,000 contracted a neurological disease called Guillain–Barré syndrome, in which the body’s immune system attacks its own nerves, causing permanent paralysis. Since then, speed has always come second to safety.
But time can be saved if you can organise people properly. "Getting the regulatory authorities to focus, to come together, to really understand the data, all of that will make a difference to the timeframe for this," says Grant. Medical advances have also sped up the process of getting a vaccine to trial safely. The Oxford team is also changing the way they work, to speed things up without sacrificing safety, says Ewer. “We’re doing a lot of things in parallel that we would ordinarily do one after the other."
But they aren’t the only team on the cusp of clinical trials.
A tobacco warehouse in Owensboro, Kentucky may seem like an odd place for a coronavirus vaccine to emanate, but we live in strange times. British American Tobacco (BAT), which some might say is a company best known for killing people, has also entered the race to save lives. “Right now, I would hope we could leave the politics of tobacco and smoking to one side," says Kingsley Wheaton, who leads marketing at BAT, "in order that we try and focus on the matter at hand right here, right now, which is solving this Covid-19 problem globally."
NEW addition to the FREE TO READ @FinancialTimes virus tracker page...
Streamgraph and stacked column charts, showing how the focus of Covid-19 deaths has switched from Asia to Europe - and now the UShttps://t.co/j59C2msmQo#dataviz #ddj #coronavirus pic.twitter.com/VInY6vRWcG— Steven Bernard (@sdbernard) April 8, 2020
A few years ago, recognising it was selling fewer cigarettes every year, BAT invested in a company called Kentucky BioProcessing, to help find new uses for the tobacco plants it was growing but which people weren't smoking. They were especially interested in a protein that could be harvested and processed as animal feed. You take a small, hardy Australian tobacco varietal, and around halfway through its growing cycle impregnate it with an antigen for the protein. It replicates at a tremendous scale. “The plant is a mini-factory, if you like,” says Wheaton.
It became clear that this might also be a way to produce vaccines quickly and cheaply. Instead of an antigen developing a feedstock protein, Kentucky BioProcessing realised they could develop the antigens of viruses. You could clone in fields, rather than Petri dishes. In 2014, as Ebola was killing people in Africa, Kentucky BioProcessing put its newly acquired company to work. Improbably, Kentucky BioProcessing developed ZMapp, an Ebola drug that the World Health Organisation concluded, in 2018, had “benefits [that] outweigh the risks” (science has since thrown doubts on its effectiveness, however).
Every year since, Kentucky BioProcessing has worked on a seasonal flu vaccine; this year's was heading into the first stage of clinical trials when the coronavirus began its rampage across the globe. Now, the business has been reoriented to aid Covid-19 vaccine development: 50 staff members are devoted to growing an antigen that can create a vaccine in tobacco plants in a matter of weeks. You extract it, purify it and – hey presto – there’s a vaccine. Results from pre-clinical trials in animals are pending, at which point it will move into clinical trials – “which may be anything from 12 to 18 months, even with a fair wind,” Wheaton says.
Not that they’re waiting that long. Even if BAT's vaccine is ineffective, its production technique could be a game-changer. “Because a pandemic is different from an epidemic, and the need for a vaccine is everywhere and at the same time, you’ve also got to think about manufacturing capacity,” says CEPI’s Grant. “If you’re thinking about developing a vaccine for an epidemic, you’re talking millions of doses of whatever it is you’ve developed. A pandemic, you’re talking about billions.”
BAT plans to start production on their vaccine even before it knows whether it works, making between one and three million a week, just in case. Wheaton is at pains to point out that if the vaccine isn’t approved, it won’t be used, “but if it turns out our candidate vaccine is the right one, it would be good to have a stockpile of these things.”
This is where research diversity becomes so important. People may look at the vast array of organisations, private companies, university laboratories and oddball developers trying to produce different vaccines simultaneously in all four corners of the world and think, What if they all worked together? Wouldn’t it get done in half the time? Not so, says Grant, whose list of teams working on a vaccine tops 90. “You are always better to have a diversified approach than you are to have a really narrow one,” she says. “You never want a single point of failure in a situation like this." With vaccines, there are too many potential failure points to count.

During the West African Ebola crisis, pharma giant Merck was one of the first to get a drug through clinical trials. Its vaccine, rVSV Zebov-GP, had 100 per cent efficacy, but a zero per cent chance of actually being used at scale; it needed to be stored at –80°C. “You try getting a vaccine supposed to be stored at –80°C out to war-torn Democratic Republic of Congo and you’ve got massive supply problems,” says Grant. Which is why it was handy there was investment in another vaccine, by Johnson & Johnson, that wasn't so temperamental.
Most drug research works on a winner-takes-all model: invent Viagra, or Minoxodil, or Oxycontin, and you get a 20-year exclusivity licence (in the US). That means you can charge as much for it as you like. Once the licence lapses, competitors can create generic versions and the price falls. With a pandemic vaccine, the rules of the marketplace make less sense. There's healthy competition, but it’s against nature, not each other.
That said, there are economic incentives at play: make the vaccine everyone wants and you can at least recoup the costs of developing it. CEPI has ploughed $23 million into the eight programmes it's supporting underway, and estimates it will cost something like $2 billion more to get three of those into clinical testing. Altruism is fuelling initial development, but at some point realism steps in. Still, any CEPI-developed vaccines won’t result in a free-for-all (the US government's reported attempts to buy German pharmaceutical group CureVac, to get at its potential coronavirus vaccine first, hint at what could happen with international cooperation). CEPI has a stringent policy on equitable access and believes that work needs to be done now at an intra-governmental level to decide a way for people who need the vaccine most, such as healthcare workers and the vulnerable, to access it first.
Regardless, developers are keen to help in any way they can. “We’re one of many in that area, but we’d also be delighted to take a candidate vaccine and become a fast-scale manufacturer through our plant-based system,” says Wheaton.
For those in the labs, competition isn't a concern. They worry about the pressure of getting a vaccine right – and getting it quickly. When I ask Ewer if the process of developing a vaccine has been stressful, she replies with one word: "Yes".
“I try not to think about it too much,” she eventually adds. She’s stopped watching the news; a regular Twitter user, she’s now shunning the app. “I had to stop engaging with it because if I think too much about it, I get really stressed. If I think too much about what happens if none of this works, then I feel a bit overwhelmed, so I’m trying to do as much as I can do in the working day and then go home and try and be a mum to my kids at home, try and keep things as normal for them as possible, because it’s weird for the family as well – as it is for everybody.”
It can be easy to forget, as we praise our scientists and our doctors, our nurses and the collective brainpower of the experts working to lead us out of this crisis, that they’re human beings, too. The risks of getting it wrong are real and they feel them every day.
“If you ask me whether I want this really quick, or I want a robust process, I would pick the safe and robust process,” says Sanicas, who worries we’re all getting caught up in the hype around 18 months to a vaccine. “I don’t want this to be just a vaccine you bring quickly to the market but we’re not sure about the long-term effects.” He thinks it’ll take two years for anything to come to fruition.
Near the end of our conversation, I ask Ewer if there’s one thing she wishes the general public – who are clamouring for a Covid-19 vaccine as eagerly as they are for sufficient testing capacity – knew about her work. I expected her to explain the challenges of the vaccine, or to caution about its progress (she believes the best case scenario is that by autumn this year the Oxford team will have evidence of the vaccine being safe and able to induce a good immune response). I didn’t expect her to answer as she did.
“I think I would like people to know there are lots of people working very, very hard on this,” she explains. “Making vaccines is difficult and it’s expensive, but there are at least 30 different groups around the world, all trying to produce a vaccine against this disease, and hopefully one of us will produce a vaccine that is effective. I don’t really mind if it’s ours or anybody else’s, but as long as one of them works, that’s the most important thing.”
She pauses for a moment, then picks up her train of thought. “As long as somebody gets there, we don’t mind if it’s us, or Moderna, or anyone else. As long as one of us gets there, and we can make enough of it quickly enough to make an impact.”
The information in this story is accurate as of the publication date. While we are attempting to keep our content as up-to-date as possible, the situation surrounding the coronavirus pandemic continues to develop rapidly, so it's possible that some information and recommendations may have changed since publishing. For any concerns and latest advice, visit the World Health Organisation. If you're in the UK, the National Health Service can also provide useful information and support, while US users can contact the Center for Disease Control and Prevention.
For more advice, visit the following recommended websites:
Like this article? Sign up to our newsletter to get more delivered straight to your inbox
You Might Also Like

 Yahoo News
Yahoo News 
