Could this documentary change the way we perceive chronic fatigue syndrome?

It has been more than 60 years since a bewildering epidemic swept through the Royal Free Hospital in north London, rendering almost 300 members of staff incapacitated and forcing the place to close for three months.
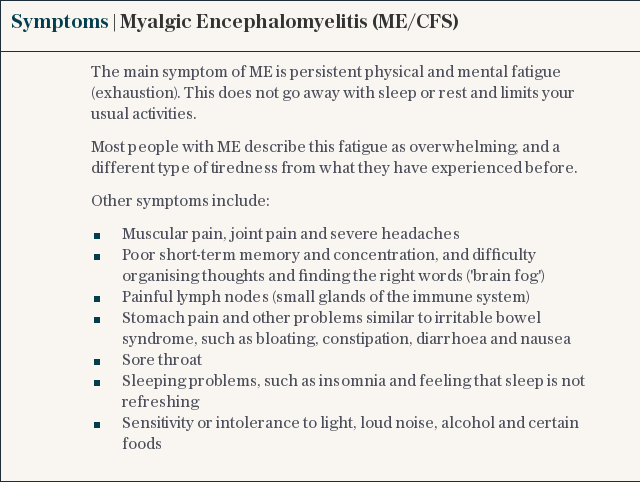
At the time, in 1955, the mysterious, polio-like outbreak (called simply ‘Royal Free disease’ for a while) had no obvious cause, certainly no cure and varying symptoms – extreme tiredness, headaches, sore throats, depression, inflammation of the spinal cord – in each victim, frustrating doctors more than it fascinated them.
In the same year, the new condition was written up in the medical journal The Lancet as “myalgic encephalomyelitis”, later shortened to ME. The mystery remained, though. By the 1980s, despite further cases having been identified all over the world, the entire Royal Free episode was put down to “hysteria”, while the illness received the dismissive nickname “yuppie flu”. At best, doctors (and employers, and friends and family, and strangers) were sceptical of victims’ insistence their problems were physiological, not psychological. At worst, they were denounced as malingerers.
Today, there are thought to be roughly 250,000 sufferers of ME – also known as chronic fatigue syndrome, though sufferers often find the word 'fatigue' does nothing to help stigma – in the UK, and more than a million in the US, the majority of whom are women, though there are likely many more undiagnosed. It’s a condition that remains starved of research funding compared to other illnesses with a similar strike rate, and incredibly difficult to diagnose or even treat, meaning the lack of understanding and empathy from the general public persists.
I realised if I could let people into homes and bedrooms and show them what it’s really like, then things would have to start to change
Jennifer Brea
Jennifer Brea, a journalist and filmmaker from New York, is one sufferer aiming to change that. In 2011, when she was a PhD student at Harvard University, Brea caught a virus while travelling with her husband, Omar Wasow, and recorded a temperature of 104F. Infection after infection followed, normally staved off by short courses of antibiotics, but her body refused to recover.
“As soon as the infection was over, I’d feel dizzy again, with increasing and worse neurological symptoms. In between, I was almost completely normal but I noticed that I couldn’t do some of the things I used to be able to do,” she says.
A keen cyclist and skier, Brea, now 35, found her threshold for exercise completely diminished. Her legs would give out on the slopes, say, or she could only do half the distance she used to. Any expenditure of energy came with a profound cost.
“I thought maybe I’m getting older. Maybe that’s what happens when happens when you’re 28, or maybe I’m out of shape.”

She became worse, to the point where she had to stay indoors, shrouded in quiet and darkness, for days or weeks. After several misdiagnoses, eventually she was finally diagnosed with ME, a chronic illness she’d never heard of.
After 18 months of being bedridden, Brea had almost completely lost the ability to read or write, turning instead to watching Netflix and surviving on the support of Wasow, an assistant professor of politics at Princeton University. A friend then suggested she keep a record of her condition by recording video and voice notes on her iPhone.
“At the beginning, it was just a place to put all of that grief and fear and anger: to process thoughts and emotions I wasn’t sharing with anyone,” she says, sitting cross-legged on a chair in a friend’s London home.
I’ve missed out on almost half of my life. In 2017, we should know about these conditions, but people are just dropping off the earth
Jessica Taylor-Bearman
Those notes turned into video clips, some taken by Wasow, to show doctors what she meant when she described being unable to speak or get up. Previously, people assumed she meant tired or tongue-tied, rather than literally incapable of moving from the floor.
“The doctor I showed the videos to went white,” she says. “I realised I needed to tell this story visually, that maybe if I could let people into [ME sufferers’] homes and bedrooms and show them what it’s really like, then things would have to start to change. Doctors don’t see us bedbound, in the middle of the night, at our worst.”
Brea’s resulting project is Unrest, a brilliant and moving new documentary telling the story of both her experience and the lives of ME sufferers all over the world. A pastiche of Skype interviews, personal confession, and expert talking heads, it’s arguably the most thorough and revealing chronicle of the ravages of ME ever made. After winning a prize at the Sundance Film Festival earlier this year, the film is now on general release in the UK, just in time for a review of the controversial National Institute for Health and Care Excellence (Nice) guidelines into the diagnosis and management of the illness.

“At its worst, ME feels like you’re being suffocated by a blanket of exhaustion,” says Jessica Taylor-Bearman, a 26-year-old author from Kent, who has suffered since she was hospitalised with a flu virus when she was 15. In Unrest, she is seen attempting to stand up for the first time in eight years.
“I’m young, and I’ve missed out on almost half of my life thanks to this. In 2017, we should know about these conditions, but people are just dropping off the earth,” she says.
At present, the Nice guidelines, established in 2010, suggest cognitive behavioural therapy (CBT) and graded exercise therapy (a gradual increase in exertion over time) as possible treatments. Both methods are fiercely criticised by patients, including by Taylor-Bearman, for whom neither has worked.
In the US, which Brea believes is well ahead of the UK in its research, both CBT and graded exercise have been repealed after studies showed they can exacerbate symptoms and cause sufferers to reach their ‘crash’ point – the energy ceiling which, once surpassed, means a patient will likely be rendered immobile for a long period of time – more quickly than before.
“I hope the UK will look at the science and update the guidelines,” says Brea, whose condition has improved considerably over the past year or two. At lunchtime today, she will present Unrest to MPs and members of the House of Lords at an event held by John Bercow at Speaker’s House. “ME patients in the UK have access to only two treatments which are, at best, ineffective and in many cases actually cause harm. There’s an urgent need to ramp up funding for biomedical research so patients have more options.”
There remains conflict in the medical world about ME having psychosomatic elements, but those who cast doubts publically are often fiercely criticised. One neurosurgeon – who refused to be named, having been professionally attacked for casting doubts before – says putting a halt to psychosomatic research is self-defeating.
“It’s becoming the case that you’re not even allowed to look into it. This remains an unexplained disorder, there’s a diagnosis based on a constellation of symptoms. Until we have a lot more proof of how the symptoms work, you have to let people look at it from all sides. It’s becoming ridiculous,” he says.
Brea, along with the academics behind numerous studies in the US, strongly dismiss that suggestion, arguing it has long been the refuge of under-pressure academics lacking clear explanation for sickness to blame the mind and soul.
“It was popular to treat cancer with therapy groups in the 70s, because they thought it was repressed anger. Then you get chemotherapy and treatments that make people better, and suddenly that argument falls away. ME – because there are no approved drugs – is one of the last bastions of that school,” Brea says.
In lieu of funding for ME-specific medicine, current trials of drugs for ME patients that are used for other illnesses, such as non-Hodgkins lymphoma and Rheumatoid Arthritis, could improve sufferers’ lives significantly, should they be proven effective.
Brea, meanwhile, puts her improvement (to the point of being able to travel and finish the film) down to two antivirals and a drug used to treat related autoimmune diseases, prescribed off-label by doctors in the US, and to the unwavering support of Wasow. She remains optimistic.
“I think we’ll eventually get drugs that can be specific to this disease, and that it’s possible I could get somewhere close to the life I used to have,” she says. “I have a lot of hope. I want to have a family. And I want to make more films. And if we invest in science, hopefully I’ll feel a lot better too.”
Unrest is in selected cinemas now

 Yahoo News
Yahoo News 