Don’t repeat mistakes of 1980s HIV crisis with Covid-19 response, UNAids warns

Millions of Covid-19 deaths could have been prevented if the world had paid more attention to the painful lessons learnt during the 1980s Aids crisis, according to experts leading global fight against HIV.
The Joint United Nations Programme on HIV/Aids (UNAids) says that the poorest and most vulnerable communities continue to be hit the hardest by the ongoing HIV global epidemic.
Its annual report warns that progress against the disease is stalling, and that the successes and failures of the global HIV response provide a blueprint for countries currently in the grip of their own coronavirus crisis.
And it advised that governments must not let private companies profit from death and despair in the race to find a coronavirus cure, as they did in the early days of HIV.
“In tackling Covid-19, we must learn the painful lessons from a history of unequal access in dealing with HIV,” UNAids chief Winnie Byanyima said. “We learnt from HIV that when companies are allowed to use intellectual property rights to monopolise their technology people die.
“Millions died of Aids-related illnesses while there were medicines available that could have saved their lives. This should not happen with Covid.”
According to the latest UNAids report, new HIV infections fell by 39 per cent between 2000 and 2019. While HIV-related deaths fell by 51 per cent over the same time period, and some 15 million lives were saved through the use of antiretroviral therapy.
However, progress towards global targets is stalling. Over the last two years, the annual number of new HIV infections has plateaued at 1.7 million and there was only a modest reduction in HIV-related death, from 730,000 in 2018 to 690,000 in 2019.
People living with HIV, and people at higher risk of infection, are facing life-threatening disruptions to health services thanks to the chaos caused by the coronavirus outbreak.
Modelling conducted on behalf of UNAIDS and the World Health Organization showed that a six-month disruption to medical supplies could result in an additional 500,000 Aids-related deaths in sub-Saharan Africa alone by the end of 2021.
While 73 countries have warned that they are at risk of supply shortages of antiretroviral medicines, such as PrEP, a drug used in HIV prevention, as a result of the Covid-19 pandemic.
“The Aids epidemic remains a global crisis fuelled by inequalities. We've been successful to reduce new infections and reduce deaths, but now with Covid disrupting the whole world, we must double down building these successes and act with greater urgency to reach the millions that are still left behind,” the UNAids head said.
Among a number of complex factors affecting the global HIV response, the report singled out gender inequality and discrimination as one of the biggest drivers of the epidemic.
In sub-Saharan Africa, young women and adolescent girls accounted for one in four new HIV infections in 2019, despite making up just 10 per cent of the total population. And there are concerns that this number will only grow as the coronavirus pandemic stretches on.
Lessons learned from the Ebola crisis show that school closures can lead to increases in gender-based violence, teenage pregnancies, child marriage, exploitation and other forms of abuse against adolescent girls (including online sexual exploitation and grooming).
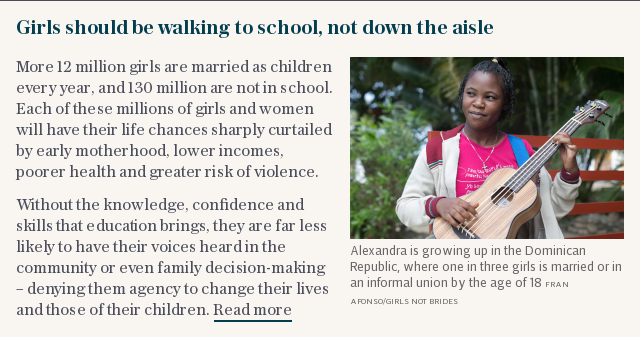
Research shows that women who experience such violence are 1.5 times more likely to acquire HIV than women who have not. While among marginalised groups, a high prevalence of violence is also linked with higher rates of infection: female sex workers have a 30-times greater risk of acquiring HIV than the general population.
For countries faced with the dual burden of HIV and Covid-19, the report found that denial, discrimination and discord continues to undermine the public health response on both fronts.
Around 62 per cent of new adult HIV infections globally in 2019 were among marginalised communities and their sexual partners.
These groups – which include sex workers, people who inject drugs, prisoners, transgender people, and gay men and other men who have sex with men – constitute small proportions of the general population, but they are at elevated risk of acquiring HIV infection, in part due to discrimination and social exclusion.
Gender inequalities, gender-based violence and the criminalisation and marginalisation of vulnerable groups continue to drive HIV forward.
However, the global response to HIV could also provide hope, said Ms Byanyima.
Of the 38 million people living with the disease, 25.4 million people are now on treatment and new HIV infections have fallen by 23 per cent since 2010, thanks in part to a substantial decrease of 38 per cent in eastern and southern Africa.
Increased access to antiretroviral therapy has averted an estimated 12.1 million Aids-related deaths since 2010 and new HIV infections have been reduced by 40 per cent since the peak in 1998.
The HIV outbreak shows that persistent epidemics can be managed, if not eliminated, and the breakthroughs in the last ten years of HIV “tell you that, where there is political will, where resources are pulled, where communities are empowered, you see progress. Rapid progress,” she said.
Protect yourself and your family by learning more about Global Health Security

 Yahoo News
Yahoo News 