The hidden health costs of lockdown
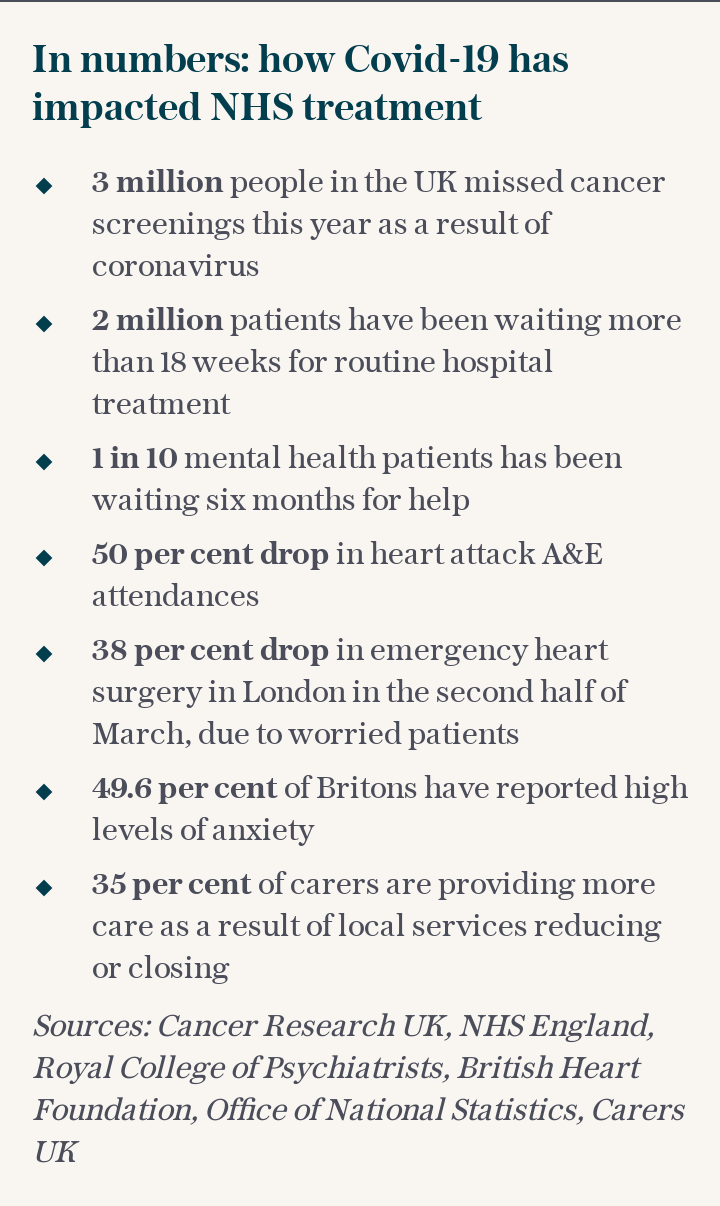
As a country we have faced more than seven months of restrictions that have seen our normal lives upended, with parts of the UK facing even tighter lockdowns. While the measures are intended to stop the spread of the deadly coronavirus, they have had – and are having – untold consequences on other areas of our health, from weight gain to delayed vital surgeries, that some experts worry could be even worse than the virus itself.
As it's reported that 50,000 people in Britain could be living with undiagnosed cancer, due to delays in NHS services, we look at the emerging picture of a country that is battling the significant hidden health costs of the Covid pandemic.
Cancer and delayed surgeries
In a new report titled The Forgotten C?, Macmillan Cancer Support have highlighted lockdown's potentially devastating impact on cancer suffers. The charity's experts say thousands of people missed out on visiting their GP or experienced disruption to treatments during the first wave of Covid – and they warn the figure of undiagnosed patients could double to 100,000 next year unless cancer services are better protected over the winter.
According to research published in the Lancet Oncology journal, delayed diagnoses and treatments from the four big cancers – breast, lung, oesophageal and bowel – alone will result in an extra 3,500 people dying in the next five years, many of whom will be young or middle aged.
Delayed routine operations
It's not just live-saving treatment that is under strain. Charities warn that delayed “routine” operations, such as on hips and knees, could lead to patients suffering for months. “Unfortunately we are now seeing patients who have severe pain and mobility issues who can now expect to wait a year or even more for their surgery, effectively sentencing them to another year of sometimes intolerable pain and disability,” says Dr Wendy Holden, Consultant Rheumatologist at the Hampshire Hospitals NHS Foundation Trust and Arthritis Action’s Medical Advisor.
Heart attacks
A new study claims that heart attacks and strokes have killed hundreds more under-65-year-olds than normal since the start of the pandemic. The research, by the British Heart Foundation (BHF), found that deaths between mid-March and May were 18pc higher than normal. Deaths also remained higher than normal during the summer.
“The coronavirus pandemic has hit heart patients doubly hard. Not only are they more at risk of severe illness and death from Covid-19, but we have also seen excess deaths from heart and circulatory disease itself. Research has uncovered effective cardiovascular treatments and these need to be provided to avoid further deaths that could be prevented,” says Dr Sonya Babu-Narayan, Associate Medical Director and consultant cardiologist.
The BHF worries that as Covid cases rise over the winter and put further pressure on the NHS, more people will die from heart problems. “Over time, heart and circulatory problems can become more urgent and delaying this care could risk avoidable harm,” Dr Babu-Narayan says. She adds that it is vital not to let a fear of going to hospital stop a person from seeking treatment.
Weight gain
With all that extra baking and snacking that we did over lockdown, around 30pc of people gained weight in spring, gaining an average of six pounds, according to Professor Tim Spector, who leads the team behind the COVID Symptom Study app. “We know from data that some people gained weight during lockdown, and that has knock on effects on our ability to fight the disease, but also on our life expectancy and susceptibility to other disease,” he says. He adds that the data shows regional differences: “Weight gain was almost double in the north of the country.”
Almost two-thirds (63pc) of adults in England are already overweight or living with obesity, according to government figures, and it is thought that excess weight puts people at greater risk of serious illness or death from Covid-19. Boris Johnson blamed his weight – 17 stone earlier this year – on how seriously he was affected by the illness and has embarked on a healthy eating and exercise regime, as well as launching a national anti-obesity strategy for the nation.
Prof Spector says there was “a clear link between drinking more and snacking more during lockdown” and weight gain. “The first thing people can do is stop grazing; there’s no such thing as a healthy snack. We should be eating less meals in a more compressed time frame to give the gut more time to relax.”
He recommends a form of intermittent fasting – restricting the hours in which you eat to between 12pm-7pm for example. “Without changing the amount you eat, just the time frame in which you eat it, you can lose weight and feel healthier,” he says.
Stress
Stress, not only from the pandemic itself, but from job losses and reduced social contact, is something Dr Natasha Bijlani, Consultant Psychiatrist at Priory’s Roehampton Hospital, feels could have “lasting consequences, not just emotional but also physical, financial and eventually to families and society as a whole. This is likely to have an adverse effect on the economic health and welfare of our nation.”
Depression and anxiety
One common symptom from stress that many of the population have felt is low mood, anxiety and even depression. “There is no doubt that these restrictions can have a detrimental impact on our moods because it can feel like the fun and enjoyment in life is being taken away from us,” says Dr Heather Bolton, clinical head of psychology at Unmind, a workplace mental health platform. Recent data from Bupa Global, the healthcare provider, found that 70pc of high net worth individuals from around the world experienced mental health symptoms since the pandemic started, with 31pc suffering from fatigue, 23pc enduring a low mood and another 23pc experiencing feelings of anger and impatience.
“A lot of people have had their social connections taken away from them, and we’re still adapting to that,” Dr Bolton says. “Or for people who have been furloughed, or perhaps don’t get the chance to help out with grandchildren, they might have had a sense of purpose taken away from them. It’s really important that we find other ways to get enjoyment from life and do things that are still meaningful to you.”
The Mental Health Foundation warns about the risk of loneliness, a feeling that has increased from one in ten of us feeling to one in four during the pandemic. It recommends joining an online class, calling a family member or friend or going for walks in public places, whilst maintaining social distancing.
Disturbed sleep
In a study conducted by King’s College London and Ipsos MORI during the spring lockdown, “half of the participants reported more disturbed, shorter sleep during the pandemic than before,” according to Dr Ivana Rosenzweig, who heads the Sleep and Brain Plasticity Centre at King’s.
Studies have shown that poor sleep can lead to long term health, problems ranging from increased risk of obesity, dementia and even cancers, to short term problems including injuries and lack of productivity. But worryingly, especially during a global pandemic, a recent study by researchers at University of Washington Health Sciences found that a lack of sleep can affect your immune system. "Seven or more hours of sleep is recommended for optimal health," said lead author Dr Nathaniel Watson.
Dental problems
There is, worries Dr Rhona Eskander, a great dental crisis that will hit the UK that has been caused by people not being able to see their dentists over lockdown. “Simple tooth decay has progressed into more severe infections and teeth that once needed simple fillings suddenly needed root canals as people were unable to see a dentist,” she says.
She adds that the problem was compounded as “more people were snacking on sugary food and drink due to stress and I saw an increase in tooth grinding and jaw pain as a result of stress.”
The problem is not over now that we can make appointments again: dentists have to allow “fallow time” between appointments, “which means there is a limit to how many patients can be seen in one day; it means we can’t see as many people as need to be seen.”
She says that one parent from Bristol “called me up in tears because their child knocked his front tooth in the garden, and they could not be seen by anyone.” She contacted a paediatric dentist colleague in London, who could fit the child in. “The family had to drive up from Bristol, but at least the teeth were seen to.”
Drink and drugs
Research by Bupa Global Wellbeing Index found that 38pc say Covid-19 increased their reliance on coping mechanisms for their mental health with crutches including alcohol and drugs. “People respond to stress in various different ways and many individuals resort to drinking alcohol and some turn to using recreational drugs as these groups of substances readily provide temporary emotional euphoria and numbing,” Dr Bijlani says. But the problem, she says, is that “regular use of alcohol makes depression and anxiety symptoms worse, reduces cognitive capacity (short and long-term), can have negative effects on memory, energy levels, behaviour and there are numerous adverse physical consequences as well.”
She says that regular intake, if drinking to relieve stress and anxiety, can quickly turn into a harmful habit leading to tolerance and dependence. She worries that there are many people who might have “slipped through the net”. “Social distancing guidelines and enforced isolation, working from home and job losses have contributed to stress levels and probably made it “easier” for some to adopt harmful coping mechanisms of drinking and drug taking without others finding out.”
Back health
Now we are all encouraged to work from home, where possible, and have left our carefully set up office workstations for huddling over a laptop at the kitchen table, experts worry about the effect this could have on our back health. “Covid has forced most of us to work at a computer station somewhere and this type of work demands being stationary out of necessity for much longer periods that one would normally undertake,” Kyle Baldwin, a Doctor of Physical Therapy from USC Department of Biokinesiology, says. He adds that he has had several patients who have come to see him recently. “They found that their pain took a couple of months to develop, and it took them another month to actually seek help.”
He adds: “Poor posture (aka slumping) ends up putting an abnormal and unnecessary stress on muscles, tendons and ligaments. Fatigue turns to pain and becomes a self-perpetuating problem. I think that people have to be more proactive than ever about their overall activity and movement to help prevent this.”
Dr Baldwin says he is encouraging his patients to wear posture-perfecting medical wear, Alignmed, which has been shown in studies to reduce fatigue by up to 29pc.

 Yahoo News
Yahoo News 
