Hundreds left with lost or damaged eyesight after NHS delays – research
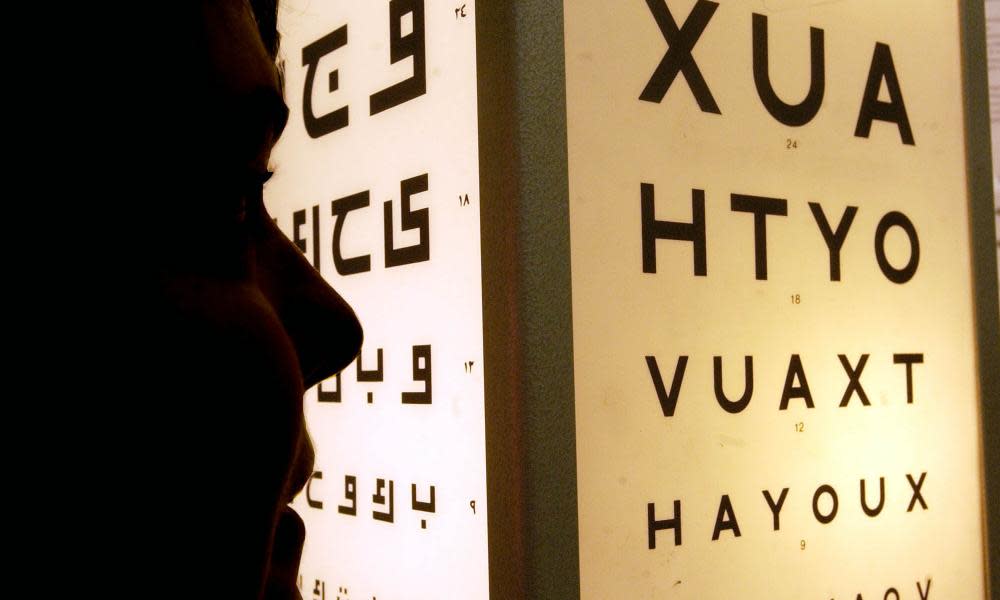
Hundreds of patients have lost their eyesight or had it irreparably damaged because of NHS backlogs, new research suggests.
NHS England clinicians have filed 551 reports of patients who lost their sight as a result of delayed appointments since 2019, with 219 resulting in “moderate or severe harm”, according to an FoI request by the Association of Optometrists, which believes that hundreds more cases are unreported.
Its chief executive, Adam Sampson, said sight loss was a “health emergency”, and urged ministers to introduce a national eye health strategy to enable high street and community optometrists to ease some of the burden on hospitals.
He said: “There are good treatments available for common age-related eye conditions like macular degeneration but many hospital trusts simply do not have the capacity to deliver services.
“Optometry is ideally placed to take away some of that burden – optometrists are already qualified to provide many of the extended services needed and are available on every high street, so patients can be treated closer to home. It’s incomprehensible and absolutely tragic that patients are waiting, losing their vision, in many parts of the country because of the way eye healthcare is commissioned.”
NHS England figures show that 628,502 people are waiting for ophthalmology appointments, the second largest backlog, equating to one in every 11 patients on an NHS waiting list, while 27,260 have been waiting a year or more.
The chief executive of eye charity, Macular Society, Cathy Yelf, said she received dozens of phone calls each month from worried patients. “People are terrified at the prospect of losing vision. The ones who contact us are the ones who are actively trying to solve the problem. We have no idea how many people sit at home, quietly losing their vision and not making a fuss about it.”
In a survey of UK optometrists, 72% said they have seen a patient in the last six months who had experienced a delay to treatment of 12 months or more, while nearly half (43%) had concerns about patients who could lose sight unnecessarily.
This is the experience of Pam Perceval-Maxwell, 75, who developed wet age-related macular degeneration in 2021 in her only good eye, which requires regular injections. The first two injections happened within a four week period, as required, but since then there have been delays of 12 and eight weeks, causing a rapid decline in her sight and an examination showed vision has been lost.
“I’m terrified I will lose my sight entirely. When your consultant stresses how important it is to have the injections on time but you can’t get an appointment it’s such a worry. I regularly call to see if there is a cancellation but I ask myself how much longer I can I cope with it,” she said.
An additional poll by the Macular Society of 498 members of the public with macular eye conditions requiring treatment in the past two years, revealed that nearly six in 10 (57%) experienced delays, and nearly half (47%) had a loss or decline in vision as a result. Four in 10 feared losing their sight, with 21% struggling with day-to-day tasks.
A Department of Health and Social Care spokesperson said: “No one should have to suffer avoidable sight loss and we are taking action to improve access to services, including appointing a national clinical director for eye care to oversee the recovery and transformation of services so patients receive the care they need.
“We are also investing in the ophthalmology workforce with more training places provided in 2022 – and even more planned for 2023 – alongside improved training for existing staff. We have made strong progress in tackling the Covid backlogs – including those waiting for eye care.”

 Yahoo News
Yahoo News 
