Monkeypox may have been circulating in UK for years, scientists say
Public health officials have confirmed seven more cases of monkeypox in England, bringing the UK total to 78, as scientists said the virus may have been circulating unseen for several years.
The sudden surge in monkeypox, which is usually found in west and central Africa, has been recorded in at least 20 countries in the past month, with more than 200 confirmed cases and dozens more under investigation.
It is the first time the disease has spread in the community outside Africa, with all previous cases associated with travel to regions where the virus is endemic or to imported animals harbouring the virus.
The largest number of confirmed cases are in the UK, where health protection teams are isolating people who test positive and their closest contacts and offering smallpox vaccinations, which are cross-protective against monkeypox. A substantial proportion of cases are among men who have sex with men (MSM).
As efforts continue to contain the outbreak, scientists are working through how the disease came to flare up in so many countries in such a short space of time. Many suspect that monkeypox was circulating at low levels, undetected, in the UK or Europe for several years before it reached the MSM community and flared up.

Prof David Heymann, who chairs a World Health Organization expert group on infectious threats to global health, said it was possible the virus entered the UK two or three years ago and spread under the radar.
Between 2018 and 2019, four confirmed cases of monkeypox arrived in the UK, all recent travellers from Nigeria. Three further cases with similar travel history arrived in 2021.
“It could hypothetically be that the virus transmission amplified from this low level of transmission when by chance it entered the population that is at present amplifying transmission,” Heymann said. He stressed it was one of many hypotheses that needed further study before any conclusions could be drawn.
Genetic studies on monkeypox viruses taken from people in the ongoing outbreak show a close resemblance to the virus that reached the UK, Israel and Singapore from Africa in 2018 and 2019. They also carry mutations that may have arisen as the virus then circulated at low levels.
While the UK’s first official case of 2022 arrived from Nigeria on 4 May, the virus was already in the country.
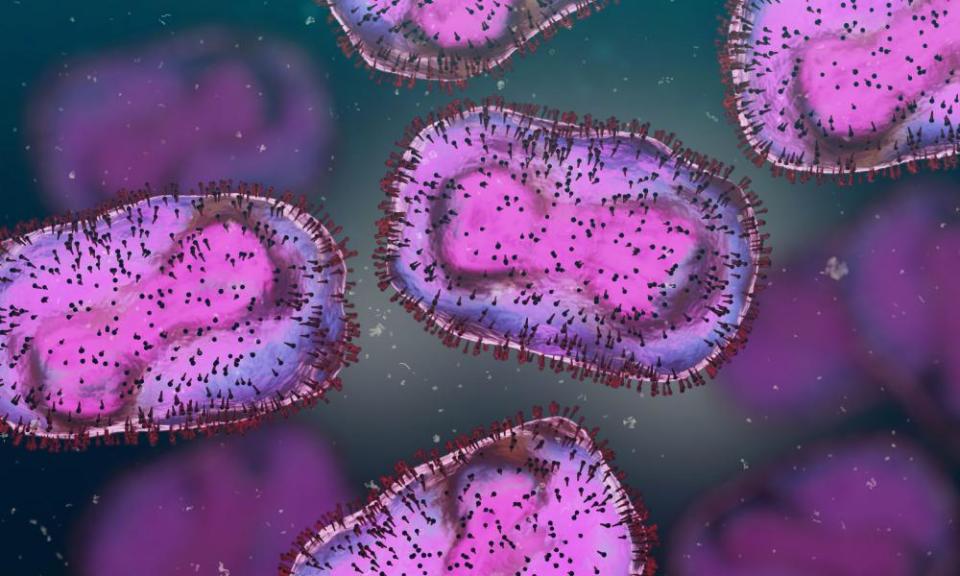
On 14 May the UK Health Security Agency (UKHSA) released images of monkeypox, and doctors in sexual health clinics realised some of their patients could have the disease. The patients had tested negative for common infections and doctors suspected a condition called disseminated gonococcal infection, before the patients tested positive for monkeypox.
“This may be a virus that’s been circulating undetected for quite a while,” said Prof Marc Van Ranst, a virologist at the University of Leuven in Belgium. “They all have a common ancestor and that common ancestor probably dates back to 2019, though it’s too early to date with any kind of accuracy.”
It is unclear whether mutations seen in the virus make the strain more transmissible in humans, but scientists point to the virus having evolved while infecting humans.
“We know that chronic infection is not a plausible scenario, and that means there has been a chain of transmission events that apparently went unnoticed,” Van Ranst said.
The Covid pandemic may have played a role, as people had less contact with GPs and other health services during the crisis. Asked if the outbreak might not have come to light if sexual health clinics had not been alerted by the first UK case, Van Ranst said: “It’s entirely possible.”
Prof Oyewale Tomori, a virologist and adviser to the Nigerian government, said more studies were needed to understand what is happening.
“Perhaps it was spreading silently within the community until we had this flare-up following some of the changes in behaviour we’ve seen,” he said.
“Between 2019 and 2020 if anybody came up with a rash in any part of Europe, you’re not going to think of monkeypox, your thought would be other diseases that cause a rash.
“And if the system misses that one case, then of course that’s an opportunity for it to spread from one person to another. I think the amplification came where you have a lot of people gathering with very close contact.”

 Yahoo News
Yahoo News 