Most countries not ready to deal with the next disease outbreak

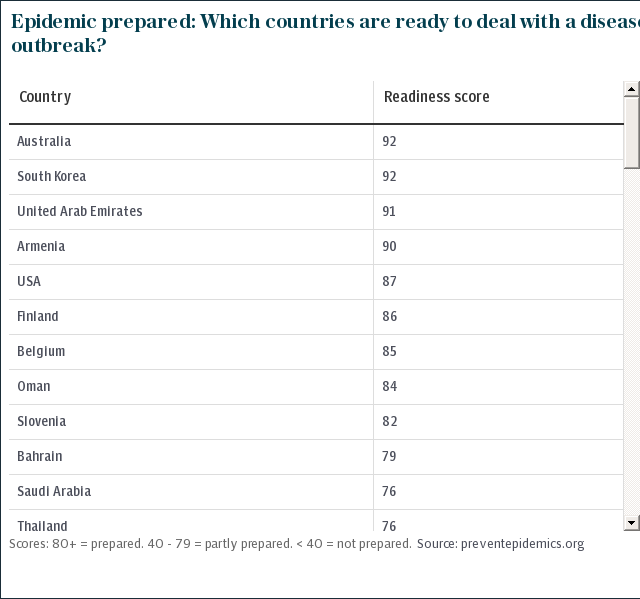
Four in five countries are not ready to detect and respond to disease epidemics and prevent them spreading beyond their borders, a new analysis has found.
The findings from the Resolve to Save Lives initiative, by US non-profit Vital Strategies, highlights which countries are falling short when it comes to readiness to respond to the next outbreak.
“Countries with lower scores are more likely to have outbreaks with preventable deaths, and that may spread to other countries,” said Dr Cyrus Shahpar, Resolve’s Prevent Epidemics director.
It is the first time that countries have been provided with a single score by international experts assessing how ready they are to prevent or nip disease outbreaks in the bud before they become full-blown crises. The scorecards published online on Thursday allow countries – and their neighbours – to see how well each nation is prepared to cope with emerging health threats.
Dr Tom Frieden, former director of the US Centers for Disease Control and Prevention and president and CEO of Resolve, said that the gaps in epidemic preparedness continue to have a life threatening impact.
“It’s not a matter of if there will be another global epidemic, but when. It’s time for the global community and countries to step up and improve preparedness," said Dr Frieden.
According to the analysis, which covers 65 countries so far, Liberia, Guinea and Sierra Leone – the three countries that were at the centre of the 2014-2016 Ebola outbreak are among those least ready to deal with an epidemic.
Nigeria, which has recently seen outbreaks of Lassa fever – a hemorrhagic illness caused by rats – and monkeypox, a rare disease that causes painful open sores, is another one of the countries that comes up poorly prepared.
The analysis is based on data that countries voluntarily provide to the World Health Organization to help them find and close the gaps in their epidemic preparedness. Almost one hundred countries are expected to have such data by the end of the year.
The USA, Australia and the UAE are among the handful of countries found to have good capacity to deal with health crises.
However, some countries that use their own assessments instead of global tools – such as the UK – are not included.

Large scale epidemics continue to pose a major threat to global health security. More than 300 new infectious diseases have been identified in the past 60 years. It can take as little as 36 hours for an epidemic to spread from a remote community to another country.
Measuring a country’s capacity through such tools is just one way to assess how ready the world is for the next outbreak, said Dr Peter Salama, WHO’s Deputy Director for Emergency Preparedness and Response. Looking at the hazards facing a specific country as well as the strength of its health system – not captured in this analysis – is also vital, he said.
“It’s also equally important to check what has happened in real life in recent years,” said Dr Salama. Nigeria, one of the countries that scored low on its preparedness has become much better at tracking risks. Many other poor-scoring countries are also continuously improving.
“These countries are on higher alert and doing better than previously,” he said. “Does it mean they are really prepared in a black and white sense? Probably not.”
According to the WHO, 80 per cent of major outbreaks begin in just 20 to 30 highly fragile countries. “This gives us a list of priority countries to focus on,” said Dr Salama. “But we also know that no country is immune from facing the consequences of major outbreaks, especially respiratory pathogens and pandemic influenza.”
Dr Shahpar said that while countries with lower scores were probably more likely to experience epidemics, it is not clear where the next pandemic will come from.
“It’s unknown, who knew H1N1 would originate in Mexico? We all must be prepared: a blind spot anywhere is risk everywhere,” he said.
Earlier this year, the UK stepped up its commitment to pandemic preparedness investing £10 million in a special WHO contingency fund that provides early emergency cash to help respond to disease outbreaks and other humanitarian health crises.
Better global and country-level preparedness was key in stopping last month’s Ebola outbreak in the DRC from spiralling into a bigger crisis, said Dr Salama. "Not only the WHO, but other key global and international actors have learned hard-won lessons from the outbreak a few years ago,” he said.
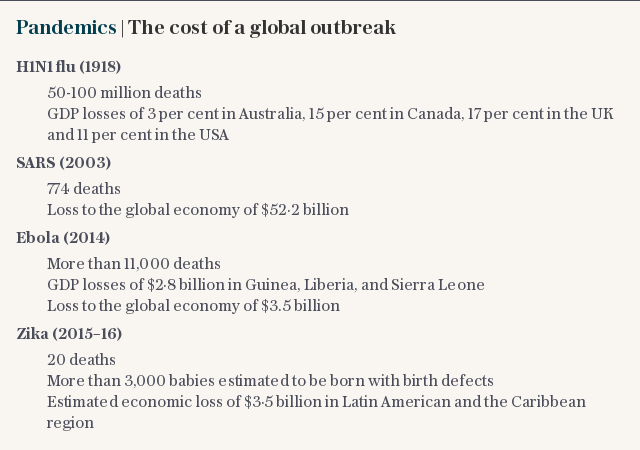
While the human cost of epidemics has gone down over the last century, the economic cost remains high. The 2014-2016 Ebola crisis in West Africa cost Guinea, Liberia and Sierra Leone $2.8 billion in lost GDP while the SARS outbreak which killed 774 people in 17 countries, led to a $52.2 billion global economic loss.
Dr Salama said however that the recent increase in urban outbreaks, such as this year’s yellow fever resurgence in Brazil, means that future epidemics could have a higher death toll.
“We are increasingly seeing disease threats in urban areas – like Rio. That’s relatively new for the world to deal with,” he said.
Protect yourself and your family by learning more about Global Health Security

 Yahoo News
Yahoo News 