‘The pandemic clock is ticking’: A race against time for a universal flu vaccine

For many people, including the elderly and others in high risk groups, getting a flu jab is a winter ritual. This year, the NHS will offer the flu vaccine to 25 million people in England – nearly half the population.
But unlike the vaccines that stop us from getting diseases like measles, mumps and whooping cough, we don’t have a single jab that can protect us against every type of flu – from the seasonal infection that kills hundreds of thousands every winter to the once-in-a-generation pandemic that can sweep across the globe in no time.
Now efforts are underway in labs around the world to develop a flu vaccine that can fight all strains of flu and be effective for years.
“The flu vaccine is better to have than not to have, but people have finally got the message that the vaccines we’ve got are not very good and we have to do better,” says Professor Sarah Gilbert of Oxford University’s Jenner Institute.
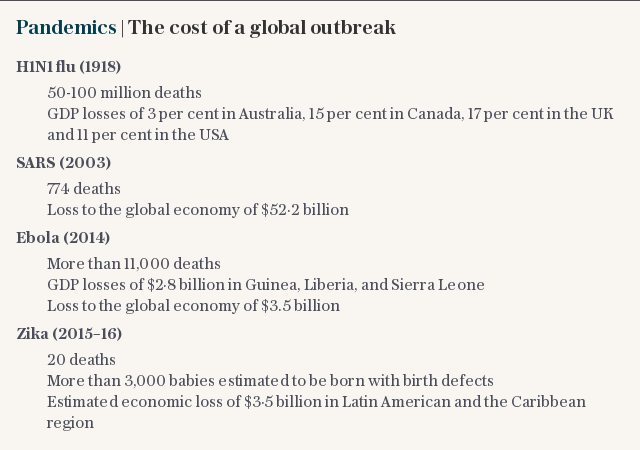
We don’t know when the next pandemic might strike but experts do agree that we are long overdue an outbreak on the scale of the 1918 Spanish flu outbreak that killed some 50 million people worldwide.
“The pandemic clock is ticking. We just don’t know how much time we have,” says Dr Michael Osterholm, who leads the Center for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota. “Right now we are not well prepared at all.”
“But each day that we don’t have a pandemic is one day more we can prepare,” he adds.
As well as being inevitable, experts agree that due to globalisation and urbanisation, a future flu pandemic could also be very destructive.
“We definitely will have a flu pandemic and it will travel around the world very quickly,” says Prof Gilbert. “It could be a catastrophe.”
Although recent breakthroughs mean we have other weapons in the flu-fighting arsenal such as a new anti-viral, baloxavir which helps relieve symptoms, preventing flu is the goal.
“The vaccine is the gold standard,” says Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases in the US, which along with the UK’s Wellcome Trust and the Bill and Melinda Gates Foundation is supporting efforts to find a better jab.
The best vaccine we currently have has to be redeveloped each year based on expert predictions of which flu strains are going to be most active during the coming winter. Depending on how good those predictions are, the vaccine can be anything from 10 per cent effective in a particularly bad year to 60 per cent effective in a good one.

As well as only being effective against specific strains, flu vaccines take up to six months to develop. This is too long when pandemics hit, says Dr Fauci.
“By the time we had a vaccine for the H1N1 strain in 2009, the pandemic had already peaked,” he says. “We need to get broader coverage so we can make a vaccine and stockpile it in the same way we do with polio or measles.”
Coming up with a universal flu vaccine will be a gradual process, according to Dr Fauci. “It will occur in a stepwise, iterative fashion,” he says. “It’s not like we don’t have a universal flu vaccine today but in a year we will.”
But although a universal vaccine is still some years off, after decades of research, experts believe we are closing in on a much-improved jab.
“I’ve seen more progress in developing a universal flu vaccine in the last three years than the last 30 years. There is very exciting research going on now in many parts of the world,” says Dr Osterholm. “It’s the most fruitful time in influenza vaccine history.”

Much of this is down to advances in vaccine design and an improved understanding of both our immune system and the tricky flu pathogen itself, including a better grasp of how the flu virus constantly mutates to evade detection by the body’s defences.
Among the scientists using this improved understanding of how flu attacks us are researchers at the Mount Sinai School of Medicine in New York.
Influenza viruses are covered in mushroom-shaped proteins known as haemagglutinin which the virus needs to bind to our cells and infect us, explains Florian Krammer, a microbiologist at Mount Sinai. “Current vaccines target the cap part of the mushroom which changes and that’s why we need to revaccinate every year,” he says.
The vaccine being developed at Mount Sinai gets around the challenge of developing an inoculation against a moving target by focusing on the mushroom’s stem which varies less from strain to strain. The vaccine is currently wrapping up a promising stage one clinical trial. If it succeeds, we could be closer to a flu shot that only has to be given two to three times in a lifetime, says Dr Krammer.
Closer to home, Prof. Gilbert is looking at an entirely different way of fighting flu using and improving on the body’s killer T cell response which destroys infected cells.
“There are two major parts of our immune system - antibodies and T cells - which are both really important in fighting infectious diseases,” she says. “Most vaccines only increase the antibody response against pathogens and ignore the protective effect of T cells, whereas natural immunity to flu uses a combination of both.”

Unlike the vaccines we currently have, the new vaccine, which is being developed by Oxford University spinoff company, Vaccitech works against a part of the flu virus that’s consistent among different strains, meaning it can protect against many seasonal types of flu as well as pandemics.
“We already know that people who have had seasonal flu are protected against pandemic flu if it comes along the following year. That’s because of T cells,” she says. “With this vaccine we’re looking to improve on that with longer immunity.”
Further down the pipeline is another potential universal vaccine candidate being developed by Israeli company BiondVax that uses a different approach again. The first universal flu jab to enter a phase 3 clinical trial, their M-001 vaccine is designed to protect against all current and future seasonal and pandemic strains using nine tiny pieces of the flu pathogen shared among many strains of the virus.
Results from the trial, which has enrolled over 12,000 people in Europe are expected in 2020.
But large trials like this are still relatively uncommon for universal flu vaccines. While increased resources particularly from public funders mean that the science is undoubtedly moving on, some scientists say funding for late-stage research – essential to bring a vaccine to market – is still a challenge.

“The money we have however, is not being spent on field trials,” says Prof Gilbert, referring to later, larger-scale trials which cost more. “New funding is mostly aimed at very early stage research.”
Some experts also worry that the economics of producing a broader flu vaccine don’t add up for pharmaceutical companies.
The current flu vaccine has to be bought and given every year, netting pharmaceutical companies billions in annual profits. This raises the question of the incentive of investing in a jab that would have to be given every few years or possibly just once or twice in a lifetime.
But doing nothing also comes at a price, says Dr Osterholm.
“One day there will be another severe pandemic like 1918 that will cost the world trillions of dollars in direct and indirect costs, not to mention the loss of millions of lives,” he says.
According to the World Bank, a severe outbreak of flu could kill 71 million people and cost the global economy $3 trillion.
Dr Osterholm says this makes for an “extremely powerful incentive” for investing in a new flu vaccine, which while expensive, would cost far less than $3 trillion.
Protect yourself and your family by learning more about Global Health Security

 Yahoo News
Yahoo News 
