Rules on isolating hospital patients are ‘crippling healthcare’, experts say

Rules on isolating people who are the contacts of confirmed Covid cases are clogging up hospital beds and “crippling healthcare”, some NHS experts have said.
Present guidance to the NHS says that inpatients who are known to have been exposed to a confirmed Covid-19 case while in hospital must be isolated or grouped together with other similarly exposed patients until 14 days after their last exposure if they remain in hospital.
This applies to all patients, irrespective of whether they have been fully vaccinated or had a previous Covid infection.
The same rule applies if the patient is discharged to a care home – they must be isolated for the remainder of the 14-day period.
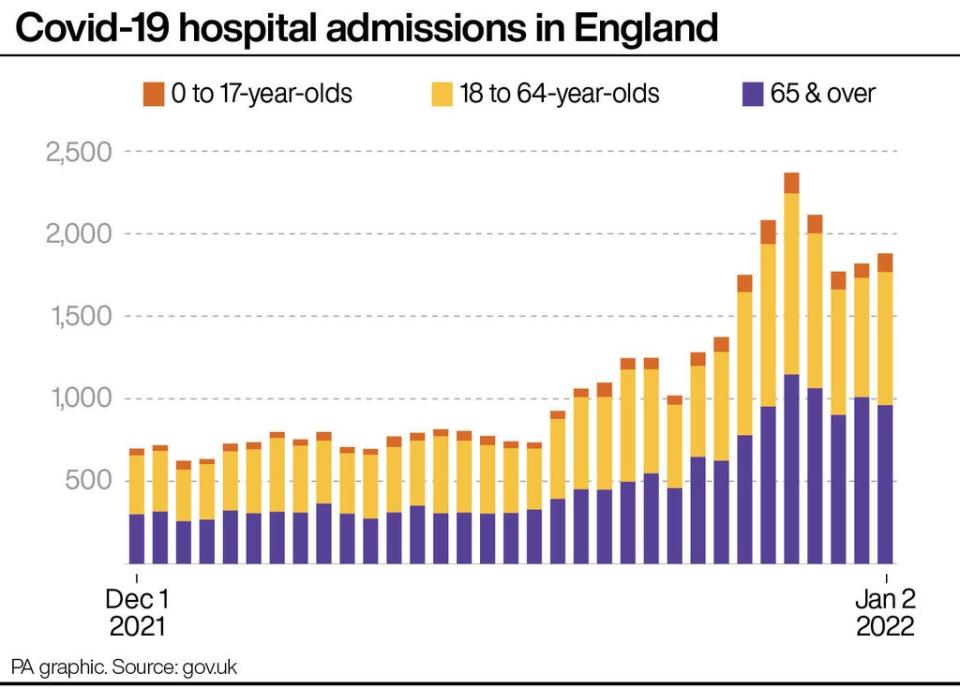
Hospitals are running out of both Covid and non-Covid capacity
London consultant
Some experts now say this is out of step with knowledge on Covid-19, the impact of vaccination, and the less harsh rules governing people exposed to Covid in the community.
They argue the current guidance is making it difficult to move patients within hospitals, is blocking discharges and tying up entire wards.
The rule was originally implemented to prevent the spread of Covid in hospitals, which caused waves of infection and death earlier in the pandemic.
The Health Service Journal (HSJ) said it understood the issue has now been raised with the UK Health Security Agency (UKHSA) and NHS England national directors.
According to the HSJ, Pat Cattini, an infection control nurse and former president of the Infection Prevention Society, said: “While in hospital [contacts] have to be isolated for 14 days. This guidance has never changed despite vaccination and changing epidemiology and is crippling healthcare.”
She called for the issue to be reviewed “urgently” and said: “This is a huge driver of bed pressure.”
A London hospital consultant added: “So many patients are turning positive at day one/two/three/four – admitted as non-Covid but incubating Covid – that it is causing devastation because of contacts and blocked beds.
“It is much, much harder to manage than Delta due to [high] infectivity… [Trusts] need to adopt different strategies and make risk assessments.”
The consultant warned that hospitals are “running out of both Covid and non-Covid capacity”.
A senior hospital consultant in another region said: “It creates another major headache for bed management as it creates another stream of patients that have to be separated.
“This headache grows when care homes won’t take patients back until they are out of the 14-day window which delays discharge.”
The UKHSA has been contacted for comment.

 Yahoo News
Yahoo News 
