Scientists discover ‘Achilles heel’ in deadly blood cancer that could boost treatment
A potential breakthrough in treating an aggressive and deadly blood cancer was announced today.
Researchers at Queen Mary University of London and in Edinburgh have discovered an “Achilles heel” in a form of leukaemia, which could open the door to less-harmful treatments.
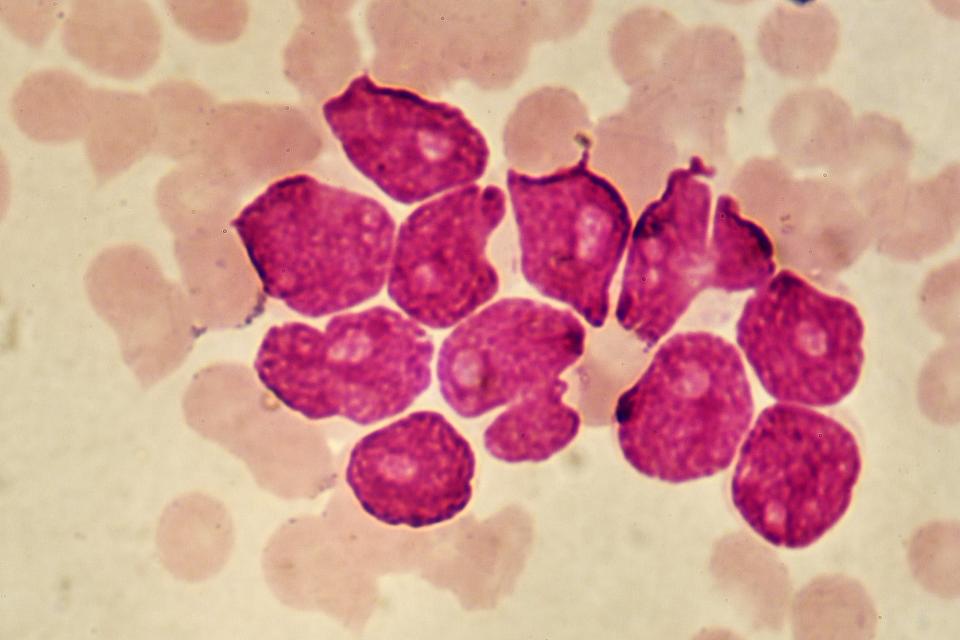
At present chemotherapy is the main treatment for acute myeloid leukaemia, a cancer of the myeloid white blood cells, which defend the body against bacterial infections.
AML is a rare cancer, affecting about 3,100 Britons a year, but mortality rates have increased almost 80 per cent since the Seventies. It is most common in people who have already undergone radiotherapy or chemotherapy, who have smoked or have blood disorders.
Researchers discovered that a protein known as YTHDF2 is needed to trigger and sustain the disease, but can be safely “knocked out” without adverse effects on the body.
This means that drugs which are able to target and eliminate the protein could improve the treatment of patients with AML. Chemotherapy is toxic to healthy blood cells, leading to damaging side effects.
The research was done in cells derived from blood donated by patients with AML, and in mice given the cancer. The tests on blood samples showed that the protein was abundant in cancer cells, while experiments in mice highlighted its role in enabling the disease to develop and survive.
The hope is that drugs can be found to remove the cancer cells without damaging healthy blood cells.
Professor Kamil Kranc from Queen Mary, who jointly led the study, said: “Our work sets the stage for therapeutic targeting of cancer stem cells.”
Professor Dónal O’Carroll, of the University of Edinburgh’s School of Biological Sciences, who co-led the research, said: “The study shows the promise of a novel class of drugs as the basis for cancer and regenerative medicine treatments.”
The study, which also involved Manchester university and Harvard Medical School, was part-funded by Cancer Research UK and published in Cell Stem Cell.

 Yahoo News
Yahoo News