Tessa Jowell wearing pioneering £240,000-a-year skull cap to treat her brain cancer
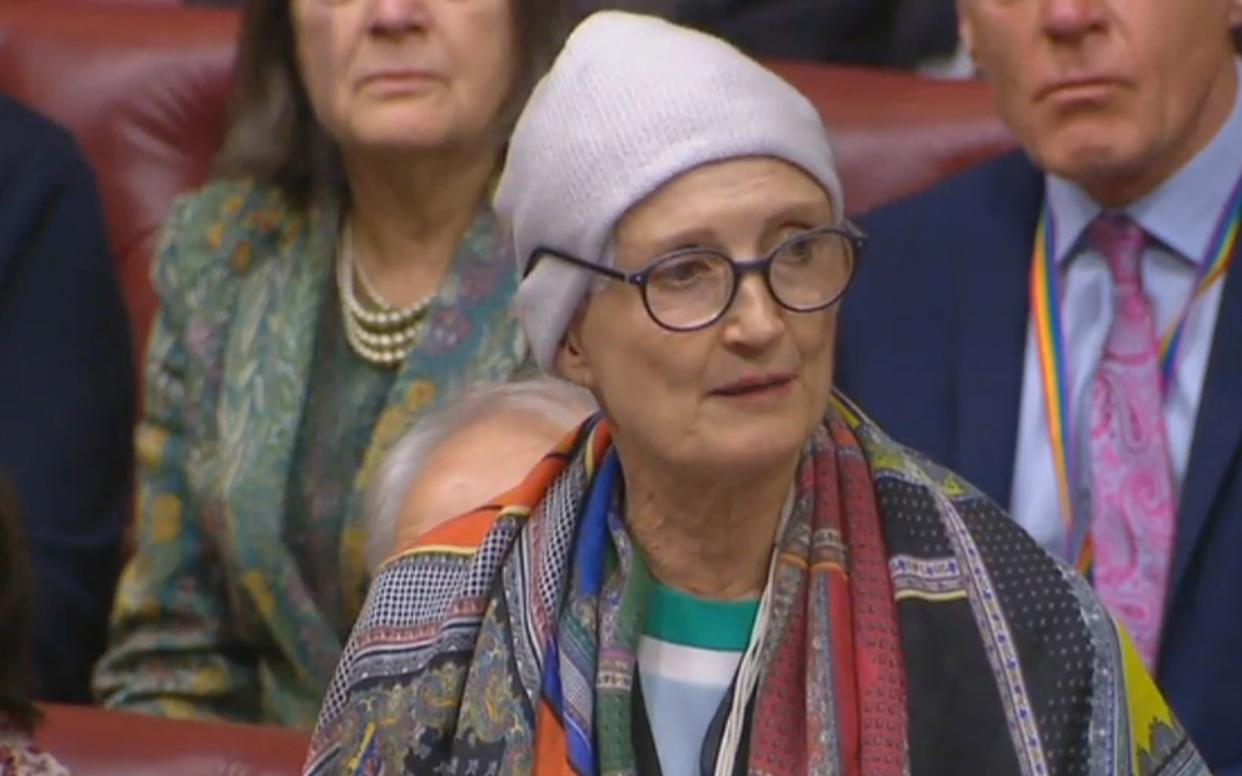
Dame Tessa Jowell has revealed she is wearing a £240,000-a-year skull cap which fires electrical pulses into her brain to treat her cancer.
The Labour peer and former Culture Secretary, who was diagnosed with an aggressive brain tumour last year, said she was wearing the pioneering device when she made her passionate speech about her condition in the House of Lords in January.
The skull cap has been provided on a test basis by the NHS, with the costs covered by the manufacturer, US firm Novacare.
However, at its current price the device is considered too expensive to be routinely offered and paid for by the health service.
The skull cap carries an array of electrodes that fire minute electrical currents into the tumour to halt the growth of cancer cells.
Dame Tessa used her Lords speech, which moved onlookers to tears, to make an impassioned call for patients to have better access to experimental treatments.
Now it has been established she herself is testing a new treatment, Optune, in an attempt to defeat her condition, a malignant glioblastoma multiforme tumour or GBM.
The high-grade tumour - which caused her to have powerful seizures - has since been removed and she has received the standard treatment of chemo- and radiotherapy, which typically has a poor prognosis.
GBM strikes 4,000 people in England every year and the average survival rate is little more than a year.
Dame Tessa has a rare mutant form of the disease that fails to respond to chemotherapy.
Whilst not a cure, Optune has dramatically improved the five-year survival rate for those who have tried it.
A clinical trial of 700 people showed that 43 per cent patients receiving Optune electrode therapy alongside the chemotherapy drug temozolomide were still alive after two years compared to 30 percent of patients treated with temozolomide alone. At five years, the survival rate was 13 percent compared to 5 percent.
Dr Matt Williams, the neuro-oncologist who is treating the Labour peer at London’s Charing Cross Hospital, said: “The device would cost £20,000 a month to rent, if we were paying for it.
“The ceramic electrodes that are attached to the scalp have to be changed every three days and we need the help of company staff who currently fly in from their European base in Switzerland.
“For the NHS to take it on board, we would have to pare down the costs.
“It takes up a lot clinic time and stretches our resources. We want to use it but we have to find a more economic model of treatment.”

 Yahoo News
Yahoo News 
