Anti-inflammatory drugs like ibuprofen and aspirin can battle major depression, scientists find

Anti-inflammatory drugs like ibuprofen and aspirin can battle major depression effectively and could be a safer alternative than antidepressants, a major new study suggests.
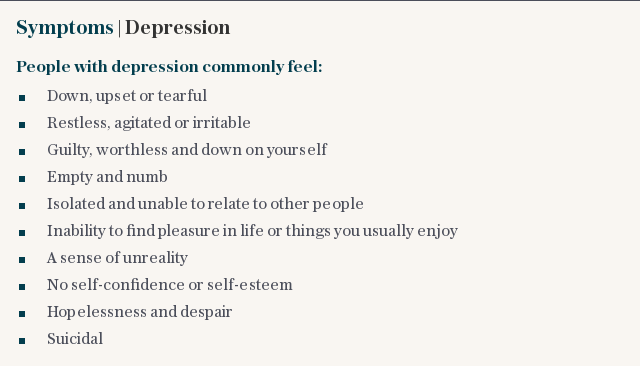
More than one in six British adults - around 7.3 million people - take antidepressants but the drugs do not work for around 30 per cent, and can bring side-effects such as nausea, insomnia, weight gain and even suicidal thoughts.
Now an analysis of 30 studies involving 1,610 people has concluded that NSAIDS (Non-steroidal anti-inflammatory drugs) were 79 per cent more effective at fighting major depression than a placebo.
Researchers at Huazhong University of Science and Technology in China, who carried out the analysis concluded that ‘anti-inflammatory agents show promising effects’ and called for long-term follow ups.
The study also found that other anti-inflammatories such as statins and omega-3 fatty acids also fight depression, and that the drugs boost the effectiveness of antidepressants when taken together.
Current treatment for depression is largely centred around restoring mood-boosting chemicals in the brain, such as serotonin, but experts now think the cause may be an overactive immune system triggering inflammation throughout the entire body which sparks feelings of hopelessness, unhappiness and fatigue.
It is similar to the low mood and that people often experience when they are fighting a virus, such as flu, and some scientists believe it is an evolutionary adaptation that kept sick people away from their family and friends.
Doctors first noticed a link between inflammation and depression and finding that people who have vaccinations often feel glum as their immune system ramps up following a jab.
Likewise, people with auto-immune conditions, such as rheumatoid arthritis, where the immune system is out of control, are far more likely to be diagnosed with depression. Several studies have reported that markers of inflammation are raised in depressed people but fall as they get better.
Professor Alan Carson, Centre for Clinical Brain Sciences, University of Edinburgh, Scotland, who edited the article which was published in the Journal of Neurology Neurosurgery & Psychiatry, said: “Depression may simply be the price we pay for having an immune system.”
The immune system triggers an inflammatory response when it feels it is under threat, sparking wide-ranging changes in the body such as increasing red blood cells, in anticipation that it may need to heal a wound soon.
Scientists believe that associated depression may have brought an evolutionary benefit to our ancestors. If an ill or wounded tribal member became depressed and withdrawn it would prevent a disease being passed on.
However a link has taken so long to establish because until recently scientists believed the brain was entirely cut off from the immune system, trapped behind the blood brain barrier.
But recent studies have shown that nerve cells in the brain are linked to immune function and one can have an impact on the other. Around 60 per cent of people referred to cardiologists with chest pain do not have a heart problem but are suffering from anxiety.
Commenting on the research, Prof Ed Bullmore, Head of Department of Psychiatry, at the University of Cambridge, said: "This should encourage further consideration of ways in which we could use a range of anti-inflammatory interventions to help people with depression, perhaps especially people who are already taking a conventional antidepressant drug with limited benefit.”
Figures also show that around 30 per cent of people suffering from inflammatory diseases such as rheumatoid arthritis are depressed - more than four times higher than the normal population.
Likewise people who are depressed after a heart attack are much more likely to suffer a second one, while the lifespan for people with cancer is hugely reduced for people with mental illness.
However Prof David Curtis, Retired Consultant Psychiatrist and Honorary Professor at UCL and QMUL, said it may be more dangerous to prescribe anti-inflammatories long term.
“Given that one would need to take treatment for several months, I don’t see that it makes sense to advocate treating depressed patients with potentially dangerous medications with at best weak effects rather than just use antidepressants, which are actually safe and effective.”

 Yahoo News
Yahoo News 
