Baby gut bacteria can help predict type 1 diabetes
A baby's gut bacteria may predict future type 1 diabetes up to two decades before the onset of the disease, scientists say.
Researchers said the findings could be used to identify those at risk of the condition, and introduce dietary changes to prevent it.
The Swedish study, which tracked children for up to two decades, found that by the age of one, the core microbiome of those who went on to develop type 1 diabetes was significantly different to that of other babies.
The group who became diabetic had far more bacteria that promote inflammation, a cause of ill-health, and far fewer health-promoting bacteria, which maintain metabolic and immune health, and keep the colon healthy.
Type 1 diabetes often arises in childhood, with an average age of diagnosis of 13.
The disease occurs when the body’s own immune system gradually destroys the pancreatic islet beta cells that make insulin.
Being able to identify gut microbial biomarkers as early as 12 months could offer prediction opportunities far earlier, allowing steps to be taken to prevent the condition, scientists said.
The Swedish research published in Diabetologia, the journal of the European Association for the Study of Diabetes, tracked 16 babies who developed type 1 diabetes with 32 who remained healthy up to the age of 20.
Average age of diagnosis is 13
Among those diagnosed with type 1 diabetes, the average age of diagnosis was 13, with the youngest aged 16 months and the oldest aged 21 years old.
Co-lead author Dr Malin Belteky from Crown Princess Victoria’s Children’s Hospital, Sweden, said: “Our findings indicate that the gut of infants who go on to develop type 1 diabetes is notably different from healthy babies and that several microbial biomarkers associated with future disease may be present as early as one year of age.”
She adds, “This discovery could be used to help identity infants at highest risk of developing type 1 diabetes before or during the first stage of disease and could offer the opportunity to bolster a healthy gut microbiome to prevent the disease from becoming established.”
Around 400,000 people are currently living with type 1 diabetes in the UK, including around 30,000 children.
Gut health
The condition is related not only to genetic predisposition, but also environmental factors such gut health and gut bacteria composition.
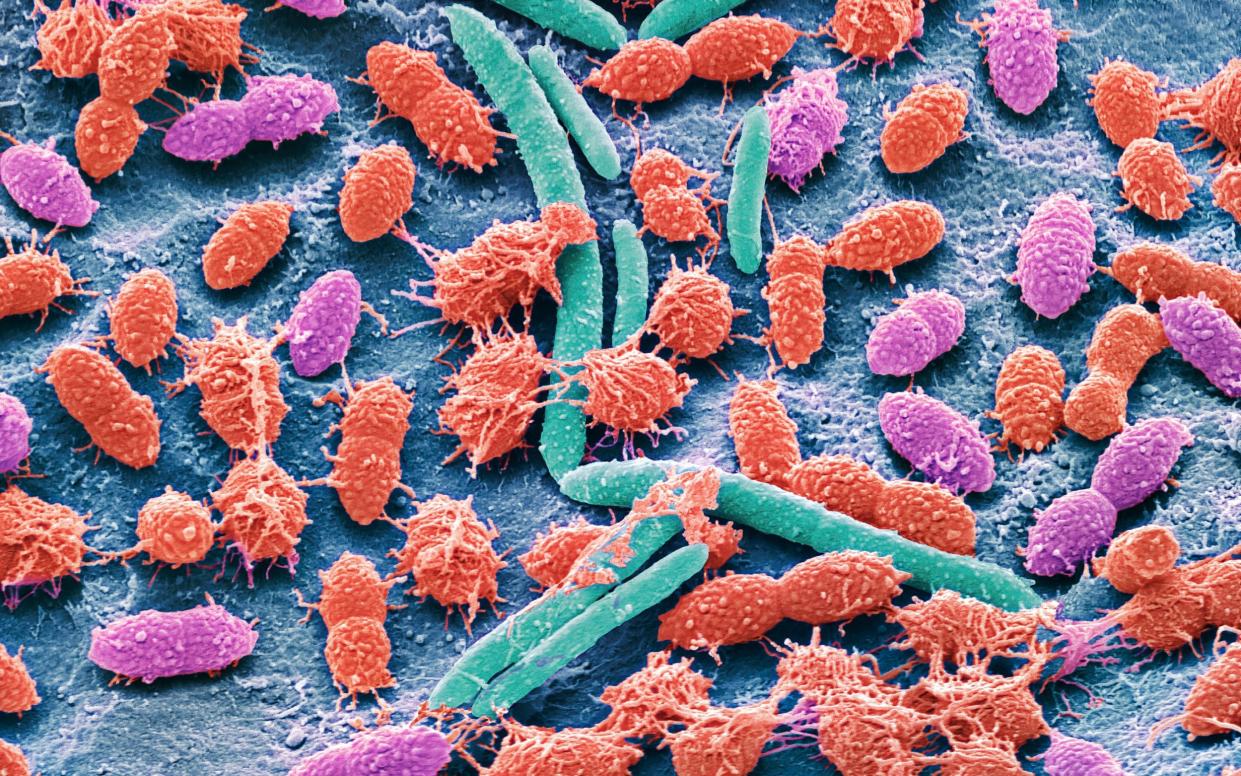
The gut’s resident microbes are already known to influence metabolism, body weight, the development of disease and the immune system.
Babies’ gut bacteria are affected by a number of factors, including how they are delivered, with those born vaginally getting most of their bacteria from their mothers, and breastmilk boosting gut health.
In the latest study, researchers tracked children participating in the longitudinal, general population All Babies In Southeast Sweden (ABIS) study, to analyse gut microbiota taken from the stool samples of babies at around the age of one.
The data was then analysed to determine which families and species of microbes were inhabiting the infant’s intestines and how the abundances of these microbes differed among samples.
The analysis found that the core microbiomes of one-year olds with a future diagnosis of type 1 diabetes were "significantly different" to that of other babies with specific bacteria identified.
Specifically, infants who went on to be diagnosed with type 1 diabetes had higher numbers of firmicutes (enterococcus, gemella and hungatella) and higher levels of bacteroides (bacteroides and porphyromonas), which promote inflammation and are known to be involved in immune response.
Health-promoting bacteria
They also had far fewer species of health-promoting bacteria compared to healthy controls, including firmicutes such as anaerostipes, flavonifractor, ruminococcaceae UBA1819 and eubacterium, which help maintain metabolic and immune health. These species produce an important short-chain fatty acid, butyrate, which helps prevent inflammation and fuels the cells of the gut lining that keeps the colon healthy.
Co-lead author Patricia L Milletich, from the University of Florida, USA, said: “Although the average age at which diabetes was diagnosed in our study was more than a decade after samples were collected, we identified distinct microbial signatures at one year of age and noted a decrease in butyrate-producing bacteria as seen in previous studies in high-risk populations,”
Co-author Professor Eric Triplett from the University of Florida, USA, “The autoimmune processes usually begin long before any clinical signs of disease appear highlighting how differences in the make-up of the infant gut microbiome could shed important light on the complex interaction between the developing immune system, environmental exposures in childhood, and autoimmunity.”
Researchers said larger studies were required to establish which are the strongest biomarkers.

 Yahoo News
Yahoo News 
