Gonorrhoea cases in England reach highest level in more than 100 years
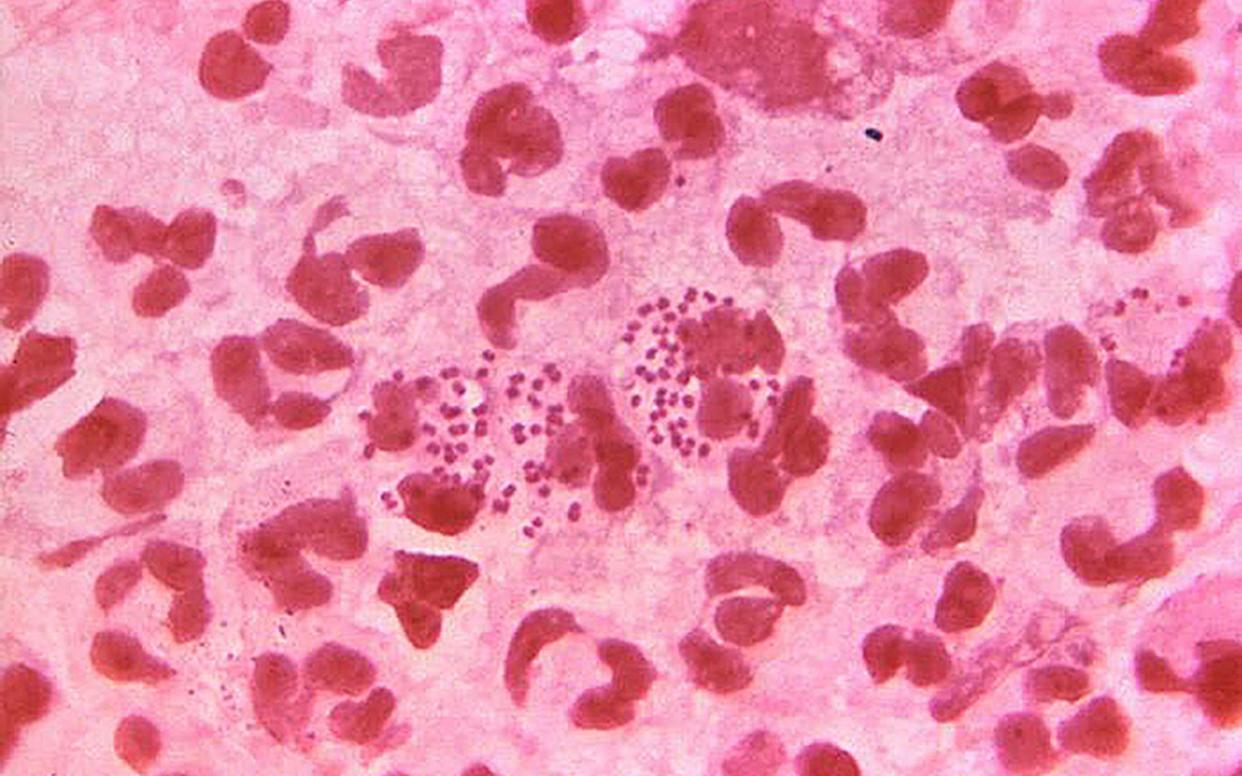
The number of gonorrhoea cases diagnosed in England in 2019 reached its highest level in more than 100 years, official data shows.
A total of 70,936 cases were reported last year, up by more than a quarter (26 per cent) from 2018.
It is the largest annual number reported since records started in 1918 and a continuation of an upward trend in recent years, according to Public Health England (PHE).
Between 2015 and 2019, diagnoses have risen by 71 per cent, from 41,382 cases to 70,936, data released on Wednesday revealed.
Overall cases of sexually transmitted infections (STIs) in England also rose last year, with 468,342 diagnoses reported, up by 5 per cent from 447,522 in 2018.
Dr Hamish Mohammed, national lead for sexually transmitted infection surveillance at PHE, said: "The considerable rise of gonorrhoea cases in England as well as the continued rise of other STIs is concerning.
"It is important to emphasise that STIs can pose serious consequences to health - both your own and that of current and future sexual partners.
"We have seen that gonorrhoea has become more resistant to antibiotics and expect to see further cases of antibiotic resistant gonorrhoea in the future, which will be challenging for healthcare professionals to manage."
PHE said the rise in STIs was likely to be due to people not using condoms correctly and consistently with new and casual partners, and an increase in testing helping improve detection of the most common infections.
Cases of syphilis rose to 7,982 in 2019, a 10 per cent increase from 7,260 the previous year.
There was a 196 per cent increase in diagnoses of Mycoplasma genitalium, rising from 1,795 to 5,311.
PHE said the rise reflects an increase in available testing following the publication of the first national guidelines for the diagnosis and management of the bacterium in 2018.
According to the NHS, Mycoplasma genitalium is the smallest known bacterium that can replicate itself.
It typically invades the cells lining the genital and urinary tracts, called epithelial cells, but has also been found in these cells in the rectum and lungs.
Mainly caught through unprotected sex, for most people an infection comes with no symptoms, but it can cause vaginal discharge and pelvic pain in women and pain while urinating for men.
Chlamydia was again the most commonly diagnosed STI, with 229,411 - or nearly half - of all new STI diagnoses in 2019.
Among young people aged 15 to 24, the number of chlamydia tests rose 2 per cent compared with 2018.
A total of 1,339,931 tests for infection were carried out in this age group - a 13 per cent decline from 2015.
The total number of consultations at sexual health services (SHSs) in England increased by 7 per cent between 2018 and 2019, from 3,613,447 to 3,852,121.
PHE officials said consultation figures "varied considerably" by service type.
The total number of consultations reported by specialist SHSs increased by 2 per cent between 2018 and 2019 (from 2,961,979 to 3,021,945), whereas the total number of consultations reported by non-specialist SHSs (excluding internet services) decreased by 10 per cent (from 390,760 to 350,064).
The number of consultations reported by internet services increased by 84 per cent between 2018 and 2019, from 260,708 to 480,112.
PHE said it is analysing data received this year to understand the impact of the Covid-19 pandemic response on the provision of HIV/STI services and the effect that social distancing measures may have had on the epidemiology of STIs.
Ian Green, chief executive of sexual health charity the Terrence Higgins Trust, said the figures revealed "the Government's ongoing inaction and lack of vision for improving the nation's sexual health".
He added: "Rates of sexually transmitted infections like gonorrhoea and syphilis are rising significantly while sexual health services are over-burdened and under-funded."
Mr Green said that as people start to have sex again as the coronavirus lockdown is eased, access to testing and treatment should be "scaled up in parallel".
He warned that while the pandemic had led to more digital services and STI testing by post, it was "not a sustainable solution for tackling soaring rates of STIs".
Mr Green said Government's plans for a national sexual health strategy "can't be delayed any further" by the pandemic.

 Yahoo News
Yahoo News 
