HRT patches, gels and tablets – which is best for you?

In all the buzz of information about the benefits of hormone replacement therapy (HRT), there is no one size fits all solution. A research review published in 2023 in the Canadian Medical Association Journal recommends HRT as a first-line treatment for menopausal women, as long as they don’t have risk factors. Official figures in 2023 show that the number of patients being prescribed HRT in England increased by almost a third in the previous year, from 1.8 million to 2.3 million.
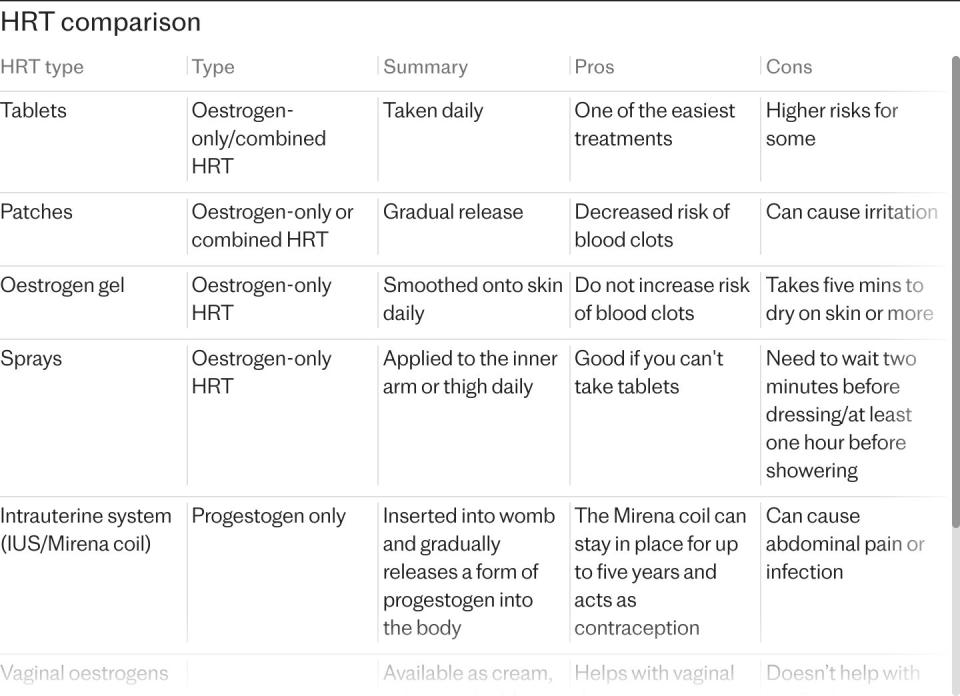
The NHS Business Services Authority (NHSBSA) says the rising numbers of women taking HRT suggests new and current patients are being prescribed an increasing number and a wider range of items. But how do you know which is right for you? HRT is taken in the form of tablets, gels, patches, sprays, creams and pessaries that contain oestrogen to tackle menopausal symptoms like hot flushes, anxiety, low mood and vaginal discomfort. Symptoms can last for more than 10 years and can reduce your quality of life. Finding the right treatment can be the difference between living well and struggling through.
Which HRT is right for you?
Medical history
“If you’re a slim, healthy young woman with no medical conditions, you could probably choose any type of HRT,” says Kathy Abernethy, a BMS menopause specialist. An older woman is more likely to have high blood pressure or cholesterol, which means avoiding tablets.
Risk of blood clots
There is a small increased risk of a clot or stroke if you take oestrogen in oral tablet form as it is metabolised in your liver, which produces clotting factors. Blood clots (or thrombosis) usually occur in your leg, and if they break off and travel to your lungs it can be serious. Some conditions can increase your risk of getting a blood clot, including some cancers and lupus, and being a smoker puts you at greater risk. “If your BMI is over 35, you’re not going to be given oestrogen tablets because of the risk of thrombosis,” says Abernethy.
Your age
“While many younger women may opt for a natural body-identical form of HRT, ie patches, gels or spray, tablets are in fact a good option as well,” says Abernethy. If you’re young and healthy, tablets are not dangerous, unlike when you’re older and have to be more cautious. “Younger people often need slightly higher doses than older ones,” she adds.
Potential duration
“If you think you’re going to be on HRT for more than five years, body-identical types, such as patches, gels or spray are potentially lower risk as they contain natural oestrogen rather than synthetic,” says Abernethy.
The types of HRT
Transdermal HRT
A study in 2013 found transdermal menopausal hormone therapy is a safer option than oral therapy. Applied to your skin in the form of patches, sprays and gels, unlike with tablets, it is not thought to come with any increased risk of blood clots, and often contains body-identical hormones, which have a better safety profile and side-effects than some other types of HRT.
Potential side effects
These can include headaches, breast tenderness, nausea, skin rashes and low mood. After three months if your symptoms do not improve, your doctor may suggest changing your dose, or type of HRT. While serious side effects are rare, it’s important to be aware of the symptoms to look out for, like sudden severe headache or vomiting, speech problems, dizziness and vision issues.
HRT patches
A lot of women like patches because they’re body-identical hormones, says Abernethy, but not everyone’s a fan. For one thing, with some patches you use a new one twice a week, which can be hard to remember. “And sometimes they don’t stick on properly. What’s more they’re visible and some women will absorb the hormone better than others,” she adds.
“Estradots are the ones that women tend to ask for because they’re only as big as a postage stamp,” says Dr Elise Dallas, a specialist in menopause care at The London General Practice and an ambassador for the Menopause Research and Education Fund. “But sometimes the plaster mark from patches can lead to local irritation.”
Any woman who still has a womb will need to take progestogen as well as oestrogen as protection against the risk of womb cancer – and some patches come with both, so that’s an advantage, although there’s no dose variation in combined patches.
HRT gels
The gel form of HRT is convenient because it’s invisible once applied, although some find it takes ages to dry. “But you can be prescribed different doses of gel. And, like patches and sprays, it doesn’t carry the risk of thrombosis. But you still have to take progesterone alongside it in table form, if you’ve got a uterus,” says Abernethy.
For better convenience, there’s Sandrina gel which comes in sachets. “It’s a small amount and absorbs really quickly, unlike Oestrogel, which comes in a pump,” says Dr Dallas.
Sprays
Working on the same principle as a patch or gel, many find HRT spray such as Lenzetto more convenient as it dries quickly and isn’t visible. “You spray it against the inside of your wrist. You can have a variety of doses and as it’s non-oral there’s no venous thrombosis risk,” says Abernethy. But as with patches and gel, you need to take progesterone alongside it.
“It feels so light and lots of people get on with it very well. And if you’re not on a high dose, it’s really well absorbed,” says Dr Dallas.
Oral HRT
HRT tablets
“Tablets are probably one of the most commonly prescribed forms of HRT and really convenient because they come in both oestrogen and progesterone – both the hormones you need. They’re the lowest cost HRT, which is good news if you’re buying them privately, and they’re convenient because you just take one a day,” says Abernethy. But the downside is the increased risk of venous thrombosis. “It’s a similar risk to that with the contraceptive pill in younger women – for most women it’s not going to be a significant risk. But if you are already at a risk of thrombosis, maybe you smoke or you’re overweight or perhaps you’re in a wheelchair, then that risk of thrombosis is increased and you shouldn’t be using tablets”.
Other types of HRT
Implants
A subcutaneous hormone implant is a tiny pellet which is inserted under the skin with a local anaesthetic. “While these were really popular 20 years ago, they are not licenced in the UK, but some people still use them via costly imports. Once we had patches and gels there was no longer a need for them,” says Abernethy.
Potential side effects
Back pain, headache, itching or pain of the vagina or genital area, thick, white vaginal discharge with mild or no odour, weight gain. These may lessen as your body adjusts.
Hormonal coil
Apart from its contraceptive effects, the Mirena coil also provides the progestogen component of HRT, used alongside oestrogen. A Mirena can minimise the unwanted effects of the PMS-type symptoms of the menopause. “Although it’s synthetic progesterone it releases so little and is very suitable for those that have might have bleeding problems at the end of their perimenopause,” says Dr Dallas. The mirena coil can be used for five years as the progesterone part of your HRT.
Potential side effects
Headaches, acne, breast soreness, irregular bleeding, mood changes and cramping or pelvic pain.
Local HRT
Vaginal tablets, pessaries, gel, rings and creams are all vaginal oestrogen, used to treat the vaginal symptoms of menopause only. “These medications protect the bladder and vagina by preventing vaginal dryness, providing relief from the discomfort of painful sex. An overactive bladder is a common menopause symptom, due partly to the lack of oestrogen in the urogenital area,” says Abernethy. As these are topical treatments, they treat local symptoms while reducing the amount of oestrogen absorbed by the body.
Potential side effects
Headaches, unexpected vaginal bleeding, vaginal discomfort or itchiness, vaginal infection, pain or discomfort in the abdomen.
Other types of HRT
Progesterone
“If you have a womb and you’re taking HRT, you’ve got to take progesterone to reduce the risk of endometrial carcinoma,” says Dallas. “A common combination offered is a transdermal oestrogen in gel or patch form and Utrogestin,” says Dr Dallas.
Potential side effects
Bloating, spots and mood swings.
Compounded bioidenticals
Some private clinics offer personalised compounded bioidentical HRT (cBHRT), making a bespoke formulation. But compounded bioidentical hormones are not regulated in the same way as conventional bioidentical HRT. The British Menopause Society warns against them, stating “cBHRT products are not recommended by the BMS. They are not evidence-based for effectiveness and safety”.
Potential side effects
There is no evidence that compounded bioidentical hormones have fewer side effects than other types of HRT.
Testosterone
Women’s testosterone production drops sharply during the menopause. The hormone influences libido and arousal, but also bone strength, cardiovascular health, cognition, energy and more. Most commonly offered as a gel, cream (to rub into your thigh), injection or implant, with careful monitoring from your doctor, testosterone can take around six months to have an effect. It should only be taken under medical supervision.
Potential side effects
While this is rare, some women feel a bit ‘wired’ at the start, and others find hair growing on the spot where the testosterone is applied.

 Yahoo News
Yahoo News 
