The incredible invention made in Wales that could transform cancer care
There is a glimmer of hope that robotics could be used to diagnose and treat lung cancer in one procedure, according to medical professionals testing the technology. The method, that was developed and made in Wales, allows doctors to target and remove nodules on the lung with millimetre precision.
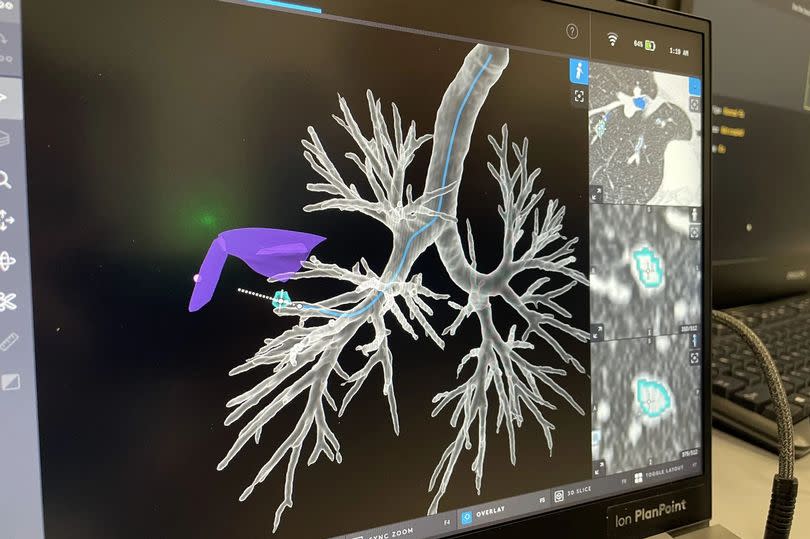
Experts have said that using robotics in this way could be "transformational" for both patients and NHS waiting lists. Prior to the procedure, a CT scan is performed and passed through software to create a detailed 3D road-map of the inside of the patient's lungs from the mouth to the location of the cancer.
A thin, robot-guided tube, or catheter, is then passed through the patient's mouth and into the airways, following this road-map. Once located, cancer cells are destroyed using heat in a process known as microwave ablation.
READ MORE: 'I was told I would die from cancer – this is everything I've learned in the 10 years since'
READ MORE: Mum-of-four 'felt like my whole world had ended' after 'terrifying' diagnosis
Professor Pallav Shah, a consultant respiratory physician based at Royal Brompton Hospital in London, told the PA news agency: "We can get to the nodule really precisely. The first patient we treated was quite interesting she had already had lung cancer and chemotherapy and radiotherapy, but then developed a spot in the radiation field. She couldn't have more radiotherapy and wasn't eligible for surgery. We had to be millimetre precise and we were. She's now over six months down the road doing really well."
The team has since treated an additional six patients. Prof Shah added: "Generally we're getting good results, but it's just early days."
Current ablation treatments require a CT scan to locate the cancer, followed by inserting a needle directly into the tumour through the skin to destroy it. This method can involve numerous ablation attempts and takes "well over an hour, maybe 90 minutes", according to Prof Shah, with a potential risk of puncturing the lung. For the latest health and Covid news, sign up to our newsletter here
The procedure being trialled by Prof Shah and his team is quicker, taking between 40 to 45 minutes overall, yet the ablation stage only requires three minutes. Navigational bronchoscopy a procedure where a narrow tube is passed through the mouth into the airways to check nodules identifies lung cancer about 65% of the time, says Prof Shah.
However, introducing robotics dramatically increases the success rate, bringing it "close to 95%", he revealed. He told PA there is "a lot of work to be done, but a lot of early promise", expressing hope that in the future, diagnosis and treatment of lung cancer could occur simultaneously.
An ongoing trial aims to treat 32 lung cancer patients who are neither fit nor eligible for surgery to gauge the safety of the procedure and the recurrence rate of cancer. The following step will be a trial using this method on patients who qualify for surgery.
The new method's safety will be compared to radiotherapy, which uses radiation to kill cancer cells but has a number of side effects. One such side effect is pneumonitis, or inflammation of the lung, which Prof Shah said can be "very unpredictable and can lead to profound damage and breathlessness".
According to the NHS, over 43,000 people each year are diagnosed with lung cancer in the UK. Smoking is the most common cause, accounting for about 70% of cases. Early detection is crucial for successful treatment. Get the best user experience with WalesOnline’s Premium app on Apple or Android.
Creo Medical, the medical device developer based in Chepstow, Wales, designed the microwave ablation tool used in the procedure. Craig Gulliford, the company's chief executive, commented: "Combining diagnosis and treatment in one procedure could potentially be transformational this reduces the need for the patient to return for a separate, more invasive procedure, which is the current standard of care.
"By removing the gap between diagnosis and treatment, it eliminates the long anxious wait for potential treatment that patients currently have to go through, but it also means that patients can get treatment before a nodule has time to grow in size or spread to other parts of the body.
"Currently, there is no early screening that takes place for cancer as there are no effective treatments for these early nodules, but this technology can allow treatment to take place earlier, at the point of diagnosis and in a less invasive manner, before these nodules become more serious."
Gulliford further implied that applying technology in such a way "could be of great benefit" in reducing NHS waiting lists.

 Yahoo News
Yahoo News 
