What to know about self-swabbing for HPV after FDA approves new kits
For the first time, women in the United States have the ability to self-collect a sample to screen for human papillomavirus (HPV).
This week, the U.S. Food and Drug Administration approved two self-swab tests from global medical technology company Becton, Dickinson and Company (BD) and pharmaceutical company Roche Holding AG for "clinical" use, meaning in a private room inside a doctor's office, mobile clinic or another health care setting.
The tests are not yet available for people to use at home.
MORE: Woman claims she got HPV-related cancer after nail salon visit
HPV is the most common sexually transmitted infection in the U.S. and can lead to several potentially deadly cancers, including cervical cancer.
Advocates hope that by having a less intrusive option, more women, especially those living in underserved areas, can get screened for HPV.
Here's what you need to know about the infection and the recently approved tests.
What is HPV?
HPV is a very common STI that infects about 13 million Americans each year, according to the Centers for Disease Control and Prevention. Nearly everyone will contract HPV at some point in their lives, the CDC says.
There are more than 100 types of HPV, and most HPV infections clear up on their own within two years.
About 10% of infections last longer and can put individuals at risk for some cancers including cervix, vaginal and vulvar cancer; penile cancer; anal cancer; and oropharyngeal cancer, which is a cancer of the back of the throat, according to the CDC.
HPV vaccine leads to more than 80% drop in infections: What parents need to know
Every year, HPV causes about 37,000 cases of cancer in both men and women in the U.S., according to the federal health agency.
How do the new tests work?
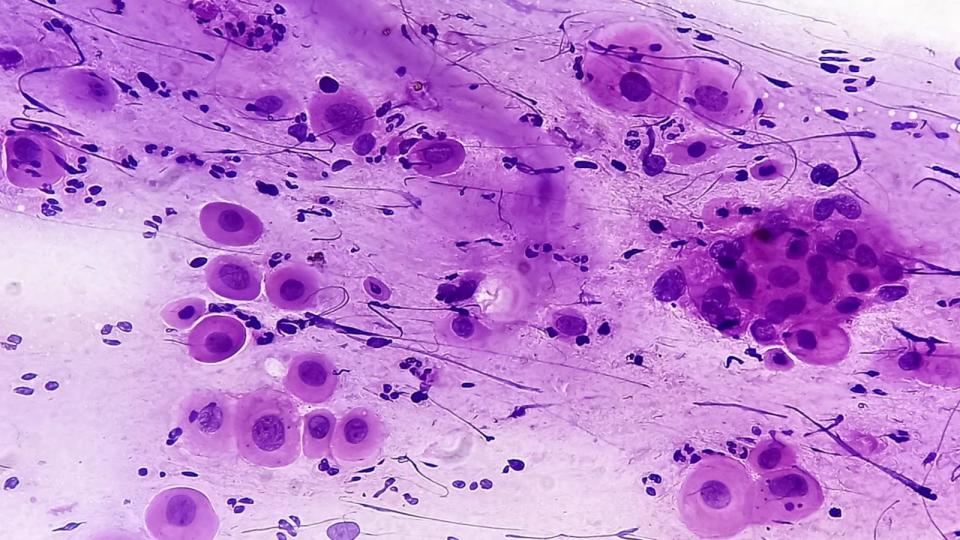
Typically, HPV tests are performed by gynecologists, who swab the cervix to collect a small sample of cells, which are then sent to a laboratory for analysis.
However, with these new tests, patients will be able to insert the swab themselves even at a primary care doctor's office. After the swabs are sent to a lab, the lab would relay results to the ordering doctor, who would then update the patient.
BD and Roche say they expect self-collection at some health care providers to be available this summer, with the companies needing three to four months to prepare and distribute kits and relevant information, officials told ABC News.

"Cervical cancer in general should be completely eradicated from this planet yet it continues to persist," Dr. Melissa Simon, an OBGYN with Northwestern University Hospital and director for the Center for Health Equity Transformation, told ABC News. "You can do it under your own control in the setting of ... and feel more safe collecting that sample."
Companies eventually want to make them available for at-home use. They say that could happen by the end of the year pending FDA approval specifically for at-home collection.
Experts say self-collection won't replace regular HPV screenings by a trained physician but they can expand access to testing and make more women comfortable with being tested.
"Many patients are uncomfortable with the intimate nature of a pelvic exam," Dr. Jeff Andrews, a board-certified gynecologist and vice president of Global Medical Affairs for Diagnostic Solutions at BD, said in a press release. "Also, many people live in areas without a local doctor or clinician trained to obtain a sample with a speculum. The option to self-collect in a clinical setting can help women overcome some of these barriers."
How do I prevent HPV?
An HPV vaccine was approved by the FDA in 2006. The CDC currently recommends children ages 11 to 12 receive two doses of the HPV vaccine, given six to 12 months apart, although children can get the vaccine start at age 9.
Anybody under age 26 can get the HPV vaccine if they have not been fully vaccinated, according to the CDC.
Health care providers less likely to offer HPV vaccination to teenage boys, study suggests
The American Cancer Society and the American College of Obstetrics and Gynecology recommends women between ages 21 and 29 be screened every three years with a Pap test.
Women ages 30 to 65 are recommended to get screened every five years with an HPV test or Pap and HPV co-test. This group can also receive a Pap test alone every three years.
Women aged 65 and older can stop testing if they do not have a history of cervical cancer or abnormal cervical cells and if their test results have been repeatedly negative within the past 10 years and the most recent test occurring within the past five years.
ABC News' Indira Khera contributed to this report.
Sejal Parekh, MD is a practicing pediatrician and a contributor to the ABC News Medical Unit.
What to know about self-swabbing for HPV after FDA approves new kits originally appeared on abcnews.go.com

 Yahoo News
Yahoo News 
