'I will find peace knowing my husband's death was avoidable. He should be here today - but we can't go back... we have to go forwards'

Dr Shivani Tanna has been working in the NHS for 18 years. ‘Everything [she] always had concerns about played out’ in the care of her husband, who died after NHS hospital failures. A passionate doctor from a circle of acclaimed medics, Dr Tanna was thrust into life ‘on the other side’ as a ‘patient and a relative’ when her husband, Professor Amit Patel, was struck by a life-threatening illness.
That experience, the devastated mum-of-two claims, ‘corroborates what [her] own patients have told [her] about the fact that, currently, the NHS is not fit for purpose’.
In the wake of her husband's death, Dr Tanna says his case reveals fundamental issues in the health service. “We have been indoctrinated as doctors, service users, and as a society in general to believe that this is a wonderful entity and we are so lucky to have a national health service," she says.
“However, nobody wants to address the elephant in the room - that it is operating on less than full staff constantly... there is so much poor practice that it’s become normalised."
READ MORE: An extraordinary doctor who should have been allowed to be an ordinary patient
Prof Patel had spent years becoming 'one of the best doctors in the UK', treating some of the most unwell cancer patients at the world-renowned Christie Hospital in Manchester. In August 2021, he was admitted to Wythenshawe Hospital after becoming gravely ill.
In almost incalculable odds, Prof Patel rapidly started to realise his life was in danger from the illness in which he had trained to be a national expert. Yet those scrambling to treat the professor admitted they 'had never heard of' the condition and would 'read about it', according to evidence heard at an inquest into his death last month.
Following weeks of fighting in the face of conflicting medical opinions and chaos on wards, Prof Patel died following NHS 'failures to provide basic medical attention', a coroner found.
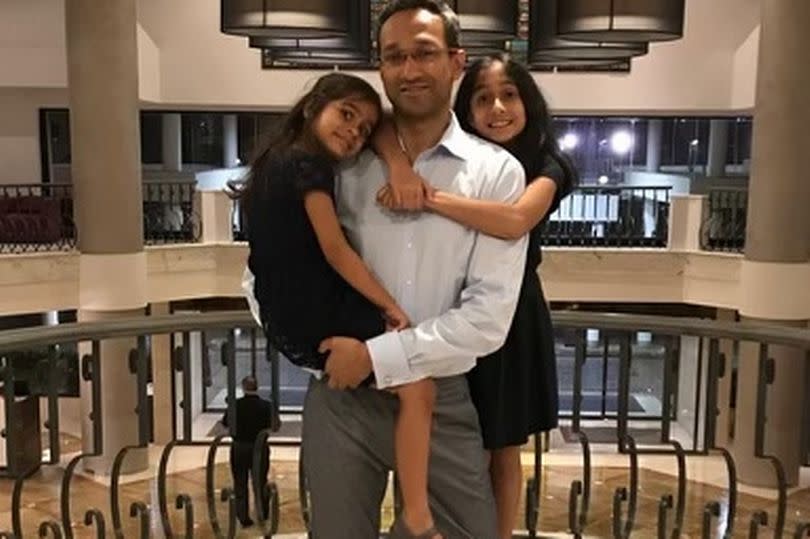
The beloved doctor and dad-of-two met a tragic death, killed by a procedure 'that should never have been recommended' by colleagues in his field and that he 'was not given the opportunity to, and therefore did not, provide informed consent' to.
Three years on and a long-running inquest to find answers later, Prof Patel’s wife is fighting to make changes to the NHS. Dr Shivani Tanna, like her husband, has long been a dedicated worker for the service. But she’s not just a doctor.
Together, the couple were raising two young daughters in Wilmslow, and loved family life together. Dr Tanna says the scenes she witnessed as a patient’s family member, while her husband was deteriorating in a Greater Manchester NHS hospital, show the major cracks in the service.
“It has not been fit for purpose for decades,” Dr Tanna told the Manchester Evening News.

"It is operating on less than full staff constantly, relying on bank staff and locums, and we’ve got doctors leaving in droves because they’ve not been nurtured or given the opportunity to work, I think, in a safe and appropriate environment.”
'He kept himself alive because he was a doctor'
Speaking in court during the inquest, Dr Tanna said the experience was 'terrifying'. She added that she feared for patients and family's without a medical background, saying: "He kept himself alive on the wards because he was a doctor – he would have been dead [within a week of him being admitted to hospital] not because he should have died, but because of sheer negligence."
Giving evidence at the inquest, Dr Tanna told the court how she had to carry out her husband’s observations as he lay on an understaffed ward, becoming gravely unwell. Prof Patel recognised he was suffering a potentially-deadly immune reaction, called hemophagocytic lymphohistiocytosis (HLH). During his career, he had formed 'national guidance' on HLH and sat on a national multi-disciplinary panel to which the most serious cases were referred.
His skills and intelligence were renowned as groundbreaking, the Manchester Coroners' Court inquest heard.
Yet when he was admitted to Wythenshawe Hospital, staff were left scrambling to treat the professor, not knowing the seriousness of the condition. Staff even told Prof Patel he was actually the least unwell person on his ward and that he didn't qualify for intensive care – despite his warnings he was suffering from a life-threatening illness.
“There were a lot of patients, a lot of shifts where you would have two nurses covering,” Dr Tanna told the M.E.N. “Even the nicest people in the world with the greatest intentions, when they are put under that level of pressure, cannot do their job.

“They physically cannot do the amount of observations they’re supposed to do. I don’t blame individuals, I blame a system where you are forced to make bad choices so that you don’t have to do the next job, which is to trigger a call to critical care outreach.
“People are being put in untenable situations in the NHS. Everyone, with the best intentions, is being pushed to do things they probably wouldn’t have done.”
The inquest heard Professor Patel had been denied access to his blood results while in hospital, despite being one of the country’s best consultant haematologists.
The GP also told of how nurses asked her to keep her husband’s fluid levels in check and do his 'basic observations' during his time on one of the Wythenshawe Hospital wards as they confessed there ‘weren’t enough staff’ to complete these tasks.
“I was doing observations on my husband because they weren’t able to do that many. That was a choice, because I could then document what was happening, and that’s important when you’re trying to figure out what’s going on with somebody,” added Dr Tanna, following the inquest.
“But there was a particular day where he had deteriorated, he really should have been on ICU before. It took a good 20 hours to get him there, but the nursing staff could not do the monitoring of urine input output.
“These are basic things that every patient should have a right to have. These are so important if you’re trying to manage people safely and carefully and you want a good outcome – but the system does not allow for that.
“The nurse that I had on that particular day was excellent, but she had seven other patients who were very unwell and probably shouldn’t have been on a general ward, and should have been escalated, but she couldn’t do anything.”
A fatal procedure that should never have recommended
Even when Prof Patel was receiving one-on-one care with some of the most senior doctors in the hospital, the coroner found stark failings.
A surgical test was recommended by that same national multi-disciplinary panel to try and diagnose the trigger for the HLH immune response, which could have been the result of tuberculosis (TB), lymphoma or, as Prof Patel suspected from an early stage, Still's disease. The endobronchial ultrasound guided biopsy (EBUS), where doctors look inside the lungs to diagnose lung disorders, could rule out TB or lymphoma – which medics decided needed to be done before giving a diagnosis of Still's, which is a rare type of inflammatory arthritis.
On May 30, coroner Zak Golombek concluded that a recommendation for a procedure from that national panel – some of whom Prof Patel knew personally – should never have happened and led to his death on October 28, 2021, aged just 43.
Ahead of the ultimately fatal procedure, test results showed Prof Patel was also suffering from disseminated intravascular coagulation (DIC). DIC is a serious and rare blood clotting disorder and can cause uncontrollable bleeding.

But Dr Jessica Manson, the consultant rheumatologist who recommended the procedure - and leader of the national-level multi-disciplinary panel which worked with Wythenshawe Hospital doctors to advise on Prof Patel's care - told the court she was never informed he was suffering from DIC, nor was Professor Patel aware he had the disorder.
Dr Manson also said she had not been informed by Wythenshawe medics there was only a small likelihood the test would provide the information needed to establish a cause for the HLH.
Nevertheless, a 'recommendation' from the MDT in this case, where doctors in Wythenshawe had little experience of treating HLH, appeared to 'send out a clear message to the treating team that an EBUS was necessary. ‘This then presented the treating team with little option but to follow the MDT’s advice', even though the panel had ‘reached their conclusion without all relevant information’, coroner Mr Golombek said during proceedings.
That surgical test was described as 'low risk'. Instead, Prof Patel ended up suffering a catastrophic haemorrhage after a blood vessel was 'transfected or ruptured' during the procedure. The chances of that happening, according to an independent expert giving evidence before the coroner, were only calculated because of this case. The witness said he'd never seen anything like it before.
The expert said the odds are estimated to be one in 10 to 15,000 cases. Prof Patel died as a result.
The coroner also found that the consenting process for Prof Patel was 'sub-optimal' when he was asked to agree to the EBUS by respiratory consultant, Dr Richard Booton. The discussion 'did not include sufficient reference to his now established DIC, and the effects that this might have on the procedure itself', the coroner said.
"The consenting process was too proximate in time to the procedure starting. This did not allow Professor Patel to compute, digest, and discuss the evolving clinical picture and the procedure itself," he added.
Prof Patel was an extraordinary doctor, the coroner told the court, but should have been allowed to be an ordinary patient.
'Poor practice has become the norm'
"Patients are made to feel grateful for a small amount of good care they receive when actually they should be entitled to excellent care,” said Dr Tanna.
“We’re a first-world country with cutting-edge research but it doesn’t translate to basic medical care that people get on a daily basis."
Returning a narrative conclusion, the coroner said: "This recommendation [of an EBUS] was based on an incomplete presentation of the deceased's clinical case, and therefore should never have been made. Had the national HLH MDT had all relevant and readily available information presented to them, the EBUS procedure would not have gone ahead on September 2, 2021, and the deceased would not have died on October 28 2021.

Mr Golombek added during the final inquest hearing: "Professor Patel was not treated like an ordinary patient. In spite of his undoubted wealth of medical knowledge, he was primarily a husband and a father, and was not given the opportunity to consider the procedure itself, and its effects on his clinical course. I got the sense from hearing the evidence that Professor Booton did not intentionally rush through the process; however, his starting assumption was that Professor Patel was fluent in the language he was speaking, and therefore did not need to spend as much time as he should have done discussing what was, in my judgement, necessary.
"This goes to the heart of the issue - Professor Booton treated this more like an academic discussion between equals, rather than a formal consenting process between doctor and patient. Thus, I find that Professor Patel was not given the opportunity to provide informed consent for the EBUS procedure on 2nd September 2021."
The coroner found the lacking consent process and mistakes of the local treating team in not passing on all relevant and available information to the HLH national panel to be 'failures to provide basic medical attention to a person in a dependent position'.
"In spite of his professional achievements and medical knowledge, he was like any other patient in a hospital who entrusted specialists with his care," Mr Golombek added.
What the trust says
The M.E.N. approached the hospital trust which runs Wythenshawe Hospital after the interview with Dr Shivani Tanna for comment on her concerns. The trust did not change its statement on the circumstances around Prof Patel's death from that which was issued immediately following the inquest's conclusion.
Jane Eddleston, joint group chief medical officer for Manchester University NHS Foundation Trust, which operates Wythenshawe Hospital, said: "We wish again to extend our condolences and deepest sympathies to Professor Patel's family at this incredibly difficult time.
"The trust has undertaken a detailed investigation thoroughly examining the care Professor Patel received when he was with us and has since shared this investigation with Professor Patel's family and the coroner.
"We are committed to providing the best care possible for our patients and we must apply the lessons learned from this to our constant work to improve our patients’ safety, quality of care, and experience."
NHS England did not respond to requests for comment.

In the wake of the tragedy, not only has the NHS lost one of its best hopes in Prof Patel, it has lost a once-staunch defender in Dr Tanna. Attending court for months, while carrying out her day job as a GP, and looking after the couple's two young daughters, Dr Tanna fought for the truth about why her husband died – and for other families failed by errors in treatment.
The failures, which she says she has lived with since her husband was admitted to hospital, and have since been borne out in court conclusions, have left Dr Tanna scarred.
“I think NHS trusts are so defensive, unwilling to accept mistakes. They talk about no-blame cultures, but that doesn’t transpire into what actually happens in hospitals and GP practices.
“It all boils down to openness, honesty. The thread in all of these cases is a defensive stance from the NHS, because there is so much poor practice that it’s become normalised and said it’s acceptable.
“I think that NHS trusts are very reactive to problems, but not proactive in terms of trying to mitigate risk. We talk about NHS values, how within a stretched, underfunded service you can then get those values to actually transpire into patient care is impossible.”
Now, Dr Tanna and her two girls face life without their guiding light. Even so, she won’t stop the fight for lessons to be learned in his memory.
“I know what happened because I was there every day with Amit during his hospital admission. The coroner found failures to provide basic medical attention to a person in a dependent position. That is enough for me.
“From the outset, I just wanted the truth to be found. I owe that to Amit. The girls will carry in on his legacy and so will I, in many ways. I’m not giving up, I’m working within the NHS, I will continue to do what I need to do to stand my ground, speak up.
“I feel for all the whistleblowers who try their best to make change. I would like Amit’s case to be the impetus for huge change in the NHS. He’s always going to be remembered throughout.
“We will find peace knowing that his death was avoidable. I know he should have been here today. But we can’t go back, we have to go forwards.”

 Yahoo News
Yahoo News 