Scots cancer patients receive less care than other countries, study shows
Cancer patients in Scotland receive less cancer care than in other comparable countries, a new study has shown.
Cancer Research UK has urged the Scottish Government to deliver on promises made in a recent strategy to tackle the disease following the study published in the Lancet Oncology.
Researchers from University College London – part of the International Cancer Benchmarking Partnership (ICBP) – studied data of more than 780,000 people between 2012 and 2017 in Australia, Canada, Norway and the UK, looking at the proportion of patients treated with chemotherapy or radiotherapy and the waiting times they face.

In Scotland, 29.3% of patients were were treated with chemotherapy – higher than only Northern Ireland where 28.8% were recorded – and 19.9% were treated with radiotherapy, the same as Northern Ireland but 0.2% higher than in England.
The UK figures were lower than the other countries studied, with 39.1% of Norwegian cancer patients being treated with chemotherapy and 22.5% with radiotherapy.
In the included Canadian provinces, 38.5% were treated with chemotherapy and 25.7% with radiotherapy and the two Australian states included – New South Wales and Victoria – boasted 42.1% and 23.9% respectively.
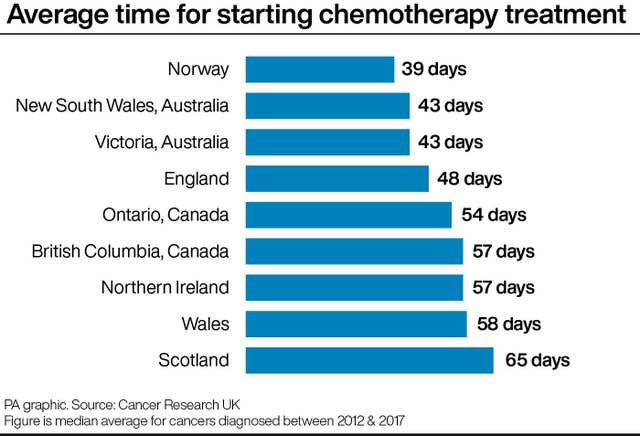
Scotland also showed the worst waiting times for chemotherapy in the UK with patients waiting on average 65 days, compared to 58 in Wales, 57 in Northern Ireland and 48 days in England.
Waiting times for chemotherapy in Scotland were higher than all but one of the surveyed regions in other countries, with those in the Saskatchewan province of Canada waiting on average 74 days, while nearby Manitoba was also on 65 days.
While waiting times for radiotherapy in Scotland was 79 days, with only Wales recording worse waiting times on 81 days.
Dr Sorcha Hume, the public affairs manager for Scotland for Cancer Research UK, said the country should be “striving for world-leading cancer care”.
She added: “The Scottish Government’s new cancer strategy promises to improve cancer survival and provide excellent, equitably accessible care for all cancer patients in Scotland so it’s crucial the Scottish Government delivers on its promises.
“A particular focus should be those set out in the strategy’s first three-year action plan, including the commitment to rolling out new pathways for patients and addressing the current workforce issues facing cancer services.”
Professor David Cameron, a deputy chairman of the ICBP and chairman of the Scottish National Systemic Anti-Cancer Therapy programme board, said: “We now need to look at our own data and see why we appear to be different, and what we can do to improve the care offered here in Scotland.”
Scottish Conservative health spokesman Dr Sandesh Gulhane said the findings were “truly horrendous”.
He said: “These damning studies expose the ticking timebomb Scotland is facing in relation to cancer cases on the SNP’s watch.
“It should be a source of shame for the SNP Government that cancer patients here are waiting much longer to start treatment and have also received less treatment in the last five years.
He called on Scotland’s Health Secretary Neil Gray to “get a grip of this crisis”, adding: “Successive SNP health secretaries have failed to meet their cancer waiting time target for well over a decade now so they cannot use the pandemic as an excuse for their dreadful record.”
A Scottish Government spokesman said: “Cancer remains a national priority for the Scottish Government and we are treating almost 50% more patients on the 62-day cancer pathway than 10 years ago.
“The 62-day standard remains challenged, however the median wait is 50 days from urgent suspicion of cancer referral to first treatment.
“We recognise that this data cover the time period between 2012 and 2017 and there has been continued improvement to services since.
“We are working with Public Health Scotland to understand whether the identified differences in the use of radiotherapy and chemotherapy in Scotland compared to other countries can be explained by the different needs, and age profile, of patients in Scotland.
“Access to treatment for cancer is vital. However, it is crucial that treatment decisions are aligned to patient choice and clinical judgment on what is best for individual patient outcomes.”

 Yahoo News
Yahoo News 
