This new treatment could make pancreatic cancer a manageable disease
Cancer is among the leading causes of death worldwide. There were approximately 14m new cases diagnosed and 8.2m cancer related deaths in 2012. This figure is expected to rise by about 70% over the next two decades.
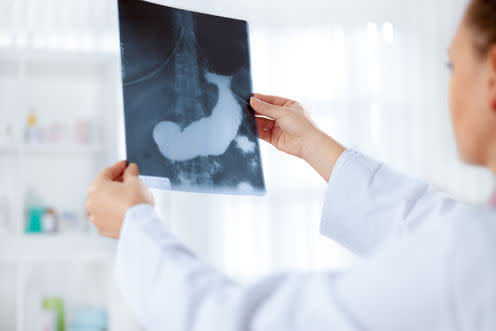
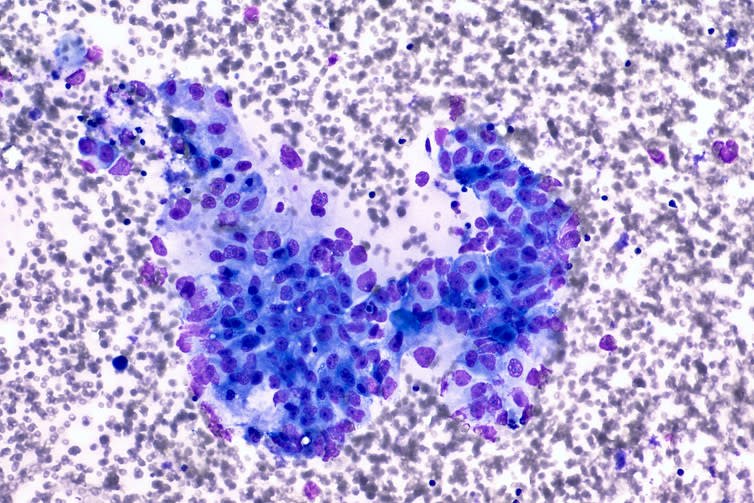
Pancreatic cancer is the eighth most common cause of cancer-related mortality worldwide, with incidence almost equalling mortality – that is, almost as many die from the disease each year as develop it. There are several types of pancreatic cancer, but more than 90% of cases are pancreatic ductal adenocarcinomas (PDAC). PDAC has one of the lowest five-year survival rates as well as a general resistance to chemotherapeutic approaches. As a result, the treatment of PDAC remains a major challenge in oncology.
There is a common theme in some of the most prolific aggressive cancers, and that is a protein known as S100P. This protein is highly expressed in pancreatic cancer and once this protein is activated it results in signalling changes that tell the cell to grow and divide remarkably quickly. This induces the cells to spread and create new cancerous growths around the body. This makes S100P a great target for developing new drugs to prevent the spread of aggressive cancers – and pancreatic cancer in particular.
Seeking a fix
Scientists at the University of Hertfordshire, in collaboration with Dr Tatjana Crnogorac-Jurcevic of Barts Cancer Institute, Queen Mary University of London, used computational chemistry methods to design new compounds that would in theory prevent S100P from being activated.
In a project funded by the charity Worldwide Cancer Research, Dr Stewart Kirton of the University of Hertfordshire designed the structures of new drugs based on Cromolyn, a drug that can be used to prevent allergy-induced asthma. These new compounds were then synthesised by Hertfordshire’s Dr Sharon Rossiter and her team of chemists. I started my PhD with the aim to identify the lead compounds that could be further developed as a suitable drug that would present the further spreading of the cancer. My supervisory team included scientists with a wide variety of disciplines: Dr Louise Mackenzie (pharmacologist), Dr Sharon Rossiter (chemist), Dr David Chau (cell biologist) and Dr Pryank Patel (biochemist), whose expertise had helped to focus my research.
I then used molecular biology techniques to screen a bank of 93 synthetic compounds for their ability to prevent the activation of S100P. From that work, 18 potential drugs were identified and then tested to see how toxic they are to cells.
The compounds themselves did not kill the cancer cells, but they did prevent them from migrating. This is an excellent profile for a drug to treat this type of cancer, since in theory any drug that worked in this way would both slow down the progression of the cancer and make it more vulnerable to chemotherapy.
The next stages are to look at ways to make sure that there are as few side effects possible by making small changes to the structure of the most promising candidate drugs. If successful, it might make a difference for patients between no survival – and a prolonged life. One day, pancreatic cancer may even become a manageable disease.
This article was originally published on The Conversation. Read the original article.

The research project at the University of Hertfordshire as a whole was originally funded by the charity Worldwide Cancer Research. The supervisory team for Deborrah Ogbeni’s PhD is: Dr Louise Mackenzie, Dr Sharon Rossiter, Dr David Chau and Dr Pryank Patel. The PhD is part of a much bigger project that originates from Dr Sharon Rossiter and Dr Stewart Kirton’s work on S100P at the University of Hertfordshire, plus a collaborator at the Barts Cancer Institute, Queen Mary University of London; Dr Tatjana Crnogorac-Jurcevic.
Louise Mackenzie does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond the academic appointment above.

 Yahoo News
Yahoo News 
