Why distancing and hand-washing won't stop the spread of Covid in schools
Since the start of the pandemic in England, discussions about Covid-19 in children and schools have been fraught. While many parents rejoiced that schools would remain open in England through its second national lockdown, some worried this would limit the effectiveness of new restrictions, while nearly half of teachers reported feeling concerned for their own safety.
Although respiratory viruses typically hit children hard, Covid-19 has had surprisingly mild effects in kids, and fewer detected cases in children also suggest that they could be less susceptible to infection than adults. Yet the actual data about Covid-19 in children is murky. In early household contact-tracing studies, younger children were less likely to be infected by family members or to be the first or “index” case. But this may have been because children infected with Covid tend to have mild or even no symptoms.
One way around this conundrum is to take a random sample of a community, testing individuals whether they have symptoms or not. A nationally representative survey in Spain found only slightly lower prevalence of the virus that causes Covid-19 in children under 10 compared to older children and young adults.
And according to recent data from the ONS infection study, which randomly samples the population each week, infection rates in England were highest in older teens and young adults, while the rate of infection among younger children was no different to that of adults. Moreover, the amount of virus found in children with Covid-19 is not consistently lower than in adults, although children may shed the virus for less time because of having a milder form of disease.
The bottom line is that children of all ages can and do contract the virus and can infect others. The susceptibility and infectiousness of younger children may be slightly lower than older age groups, but this apparent protection fades for teens and young adults, who contract and transmit the virus at high rates.
As schools have reopened around the world, clusters of cases have been detected, but it’s often difficult to identify whether transmission is occurring in school, at home, or in the community. Outbreaks are more common in secondary compared to primary schools, and one analysis of school re-openings in England in June found that most cases were between staff, rather than between students. But recent ONS data show that Covid-19 positivity rates in schoolteachers were no higher than in other professions.
So while it seems that transmission in schools reflects levels of community transmission rather than accelerating it, the jury is still out. What we do know is that the costs of school closures are immense. Many students lost out on education during England’s first lockdown, with disadvantaged children suffering the most. Keeping schools open and safe should be one of society’s chief priorities during this pandemic.
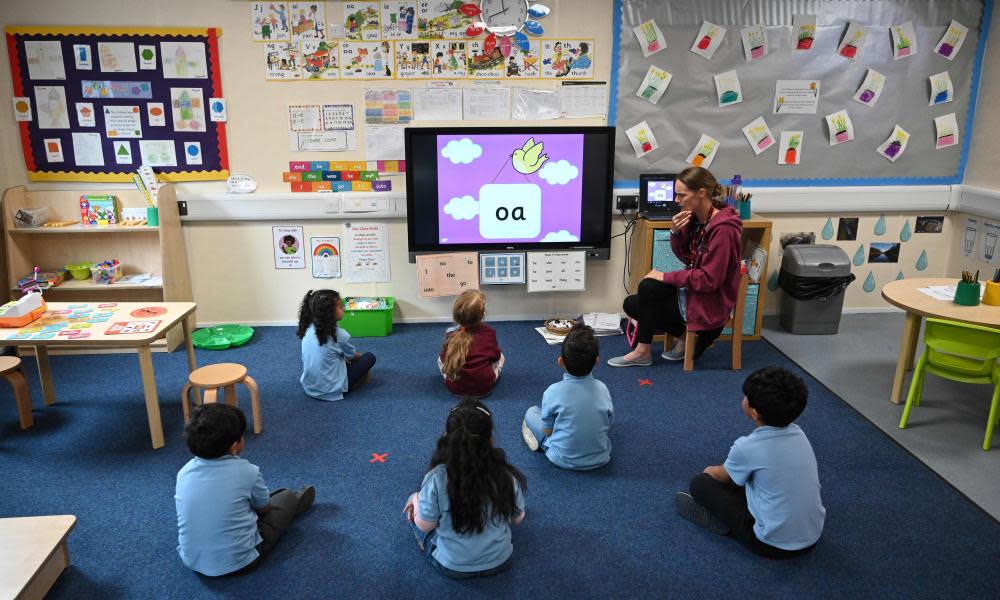
Although England has prioritised keeping schools open during its second wave, the government risks sabotaging these efforts unless it also embraces the current consensus on how to minimise transmission in schools. Children are not immune to transmission, and schools are largely indoor environments where students and staff spend many hours a day talking and interacting in close proximity – exactly the conditions in which the virus can spread.
To defeat Covid, we need to use all the tools in our public-health toolkit. While any single tactic may have weaknesses, these layers of defence become strong when stacked together. Early in the pandemic, a focus on handwashing and disinfecting surfaces dominated the prevention narrative. This “hygiene theatre” may soothe our anxieties, but it can ultimately detract from more important modes of transmission on which we should be focusing.
For example, we’ve learned that surface transmission plays less of a role in the spread of the virus compared to droplets and aerosols. And viral loads are highest just prior to the onset of symptoms – meaning that asymptomatic transmission is Covid’s superpower.
Because of this, talking may be a more significant route of infection than sneezing or coughing. Not only do people normally refrain from coughing on others, particularly if they have other Covid symptoms, but when a person talks or breathes, the virus hitches a ride on the small particles they emit. Larger droplets produced when coughing or sneezing usually fall to the ground within a 1- or 2-metre distance, whereas smaller aerosols float over larger distances and can accumulate in indoor spaces, much like smoke. This reduces the benefit of a “catch it, bin it, kill it” approach.
Recent simulations published by El País, based on the work of aerosol scientist Dr Jose-Luis Jiménez, showed how transmission occurs in different scenarios, including at school. In these simulations, people sat 2 metres away from one another, but all of the other preventive measures, including ventilating the room, shortening encounters, reducing the number of participants and wearing face masks, were needed to prevent transmission. While there are some caveats about the precision of these estimates, their conclusions are clear: distance alone can’t protect you indoors.
Although schools have already implemented some important precautions, other tools are still under-utilised. Measures such as better ventilation and universal masking are crucial. Opening windows even a few centimetres can increase the air exchange that dilutes virus-laden aerosols, while portable air cleaners with Hepa filters can capture airborne viral particles. And getting students outside as much as possible, including using tents or other structures, can also help mitigate indoor risks.
In England, the government’s current guidance on face masks in schools recommends only that they be worn by secondary school students in corridors and communal spaces. This overlooks the risk of aerosol transmission taking place over longer periods of time in classrooms. Face masks can help to physically block aerosols, and young children in schools all over the world have embraced them with fewer complaints than those heard from many adults. Younger children could be given periodic mask breaks outdoors, and here, again, the perfect need not be the enemy of the good: less than 100% masking would still make a substantial impact on reducing transmission.
It’s clear that physical distancing and handwashing alone aren’t enough to protect students and staff from indoor transmission of the virus. To get the most out of the lockdown while maintaining children’s health and education, we should help schools to embrace important prevention measures, so they aren’t fighting the virus with one arm tied behind their back.
• Jennifer Dowd is a professor of demography and population health at the University of Oxford

 Yahoo News
Yahoo News 
