New drug combination offers ovarian cancer breakthrough
Thousands of women with ovarian cancer could benefit from a revolutionary drug combination after it was shown to significantly shrink tumours in almost half of patients with the disease.
The new treatment blocks tumour growth, helping keep the disease at bay for years. Experts said the “fantastic” and “very exciting” results from clinical trials of the drug combination, presented at the world’s largest cancer conference this weekend, showed it was “far more effective” than any available option for patients.
One patient who benefited told how doctors had warned her there was nothing they could do after her ovarian cancer resisted both chemotherapy and hormone therapy.
But the breakthrough treatment has now helped her beat the disease for a second time. Her tumours have been obliterated, while the latest scan results show no evidence of disease.
The phase 2 trial, led by the Royal Marsden NHS Foundation Trust and the Institute of Cancer Research, London, tested the drug avutometinib alone and in combination with defactinib in 29 patients.
Trial results show almost half the patients on the new drug combination – 45% – saw their tumours shrink significantly. It proved to be almost twice as effective as the next best treatment – trametinib, which has a response rate of 26%.
The outcomes were even better in patients with a particular mutation, with 60% who have KRAS-driven ovarian tumours seeing them shrink after treatment.
However, nearly a third – 29% – of patients without the mutation also had an encouraging response, which is also an improvement on standard treatment.
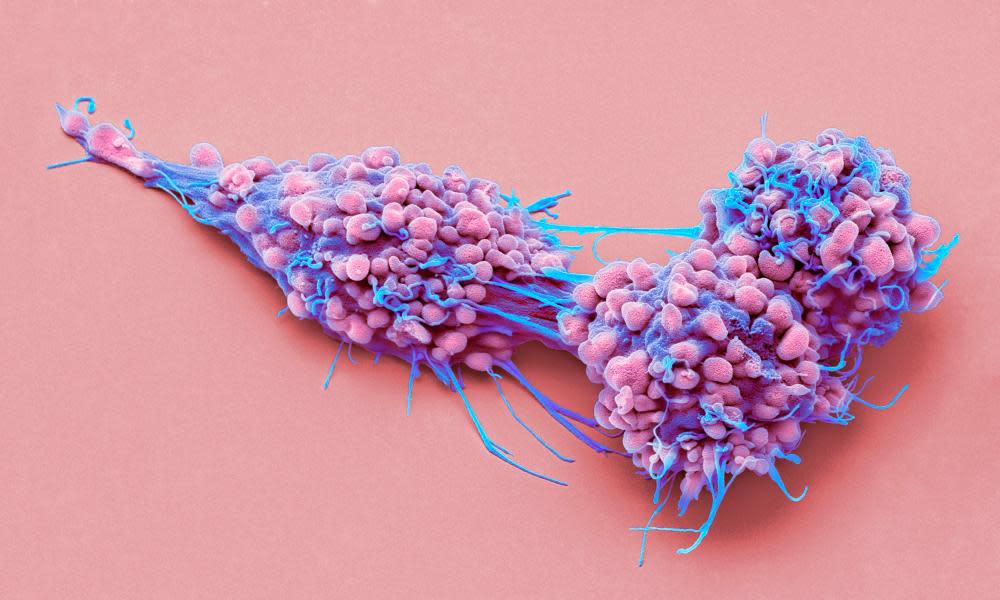
All the patients had low-grade serous ovarian cancer, which tends to affect younger women.
Dr Susana Banerjee, the global lead investigator of the study presented at the American Society of Clinical Oncology’s annual meeting in Chicago, said it could represent a “significant breakthrough”.
“These initial results could be fantastic news for women with low-grade serous ovarian cancer, indicating a far more effective option than current treatments,” she said.
Banerjee, a consultant medical oncologist at the Royal Marsden and team leader in women’s cancers at the Institute of Cancer Research, added: “It’s wonderful to see so many patients experience a meaningful response to this innovative drug combination and I’m so grateful to all who joined the trial, making this research possible.”
Avutometinib is a dual RAF and MEK inhibitor, a type of targeted drug that blocks certain proteins that help control cancer growth and survival. Studies have shown the drug can become ineffective over time as tumours develop resistance to treatment.
However, when combined with defactinib – which combats a protein that encourages drug resistance – avutometinib works more efficiently. The drug combination is over four times more effective than avutometinib alone.
Study co-author Dr Kathleen Moore, of the Stephenson Cancer Centre in Oklahoma, said the results of the new treatment were “very exciting”. “The beauty of the combination is that you’re outsmarting two ways that these tumours become resistant,” she said. “This response rate is the best ever reported for any medicine in LGSOC. This is an area of high unmet need that deserves a lot of attention.”
While survival data is not yet available from the new study presented in Chicago, previous studies indicate patients live an average of 23 months following treatment with this drug combination before their cancer progresses.
“Low-grade serous ovarian cancer does not respond well to currently approved treatments, so these results could represent a significant breakthrough,” said Banerjee. She said she was “hopeful” the results would lead to the drug combination becoming “a standard of care for women”.Originally diagnosed with low-grade serous ovarian cancer in 2009, Christine Cull, 71, was horrified to discover the disease had returned in 2014. She was treated with chemotherapy and hormone therapy, which didn’t work, along with several surgeries.
“My lowest point throughout this experience was in 2019 when my local hospital said there was nothing more they could do for me – it was horrible,” she said. “My cancer had completely resisted chemotherapy and hormone therapy, and my team weren’t able to operate again.
“Fortunately, my doctor referred me to the Royal Marsden who, as specialist cancer centre, had the expertise to do another surgery. When the disease started growing again the next year, this trial had opened at the hospital, and I was chuffed to be able to join.” Cull has been treated with the new drug combination since 2020.
“I have scans every three months and each time we’ve seen the cancer getting smaller and smaller. After finding out recently that the cancer is currently not even visible on scans, I felt relieved, amazed and so happy to be able to pass this good news on to family and friends.”
Cull, from Coventry, said the breakthrough had given her and her family hope when she thought all her options had been exhausted. “Because of this trial, I’m able to live my life with my husband, three children and three grandchildren – with barely any side effects,” she said.

 Yahoo News
Yahoo News 
