Gosport: NHS 'blame culture' must end to prevent more hospital scandals, warns Jeremy Hunt

An NHS "blame culture" must change to help prevent repeats of the Gosport War Memorial Hospital scandal, Jeremy Hunt has warned.
The Health Secretary said there is "a long way to go" to ensure doctors and nurses do not fear they will be fired for blowing the whistle.
He said he wanted to foster a "learning culture", the day after a damning report concluded a hospital GP presided over an "institutionalised regime" that saw more than 600 patients have their lives cut short after they were prescribed powerful painkillers without medical justification.
Dr Jane Barton was held responsible for policies that led to the deaths of up to 656 mostly elderly people at Gosport while she worked there between 1988 and 2000.
The report said that there was "disregard for human life" and it told how patients who were viewed as a "nuisance" were given drugs on syringe drivers that killed them within days.

It found that more than 450 people had their lives shortened after being prescribed powerful painkillers at the hospital, adding that an additional 200 patients were "probably" similarly administered with opioids without medical justification.
Families of the dead urged the authorities to bring criminal prosecutions. Speaking in the Commons on Wednesday, Mr Hunt said the police and Crown Prosecution Service would “carefully examine” if new charges should be brought.
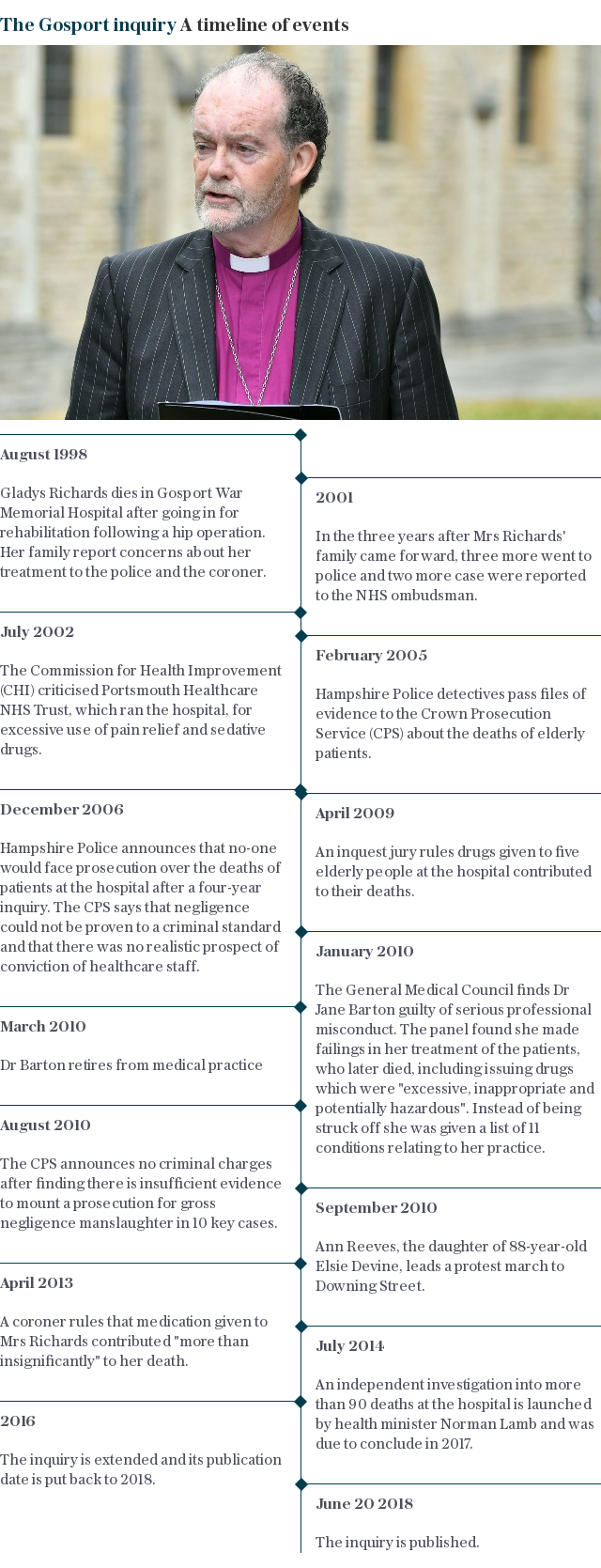
The inquiry, led by the former bishop of Liverpool, the Rt Rev James Jones, found that whistleblowers and families were ignored as they attempted to raise concerns about the administration of opioids at the hospital.
Nursing staff first raised concerns nearly 30 years ago but their fears were "silenced" by management, it revealed.

Speaking on Thursday, Mr Hunt told BBC Radio 4's Today programme: "I think there is a blame culture in a lot of the NHS."
The culture "is changing but it has got a long way to go", he acknowledged.
"The basic problem is that if you are a doctor or a nurse and you see something going wrong - even if you are perhaps responsible for a mistake yourself - the most important thing, the thing that families want if they are bereaved or if they have a tragedy, is to know that the NHS isn't going to make that mistake again.
"We make it much too hard for doctors and nurses to do that - they are worried that there will be litigation, they will go up in front of the GMC or NMC, the reputation of their unit - in some places they are worried they might get fired, so we do have to tackle that blame culture and turn that into a learning culture."
Video: Jeremy Hunt addresses Commons over scandal
Mr Hunt added: "In an organisation of 1.4 million people, unfortunately you are going to get malpractice, you are going to get some people who do the wrong thing.
"You can never say that that will be totally eliminated but I do think we would find out about that much, much sooner these days with all the things we have put in place."
The panel found that, over a 12-year period as clinical assistant, Dr Barton was "responsible for the practice of prescribing which prevailed on the wards".
The panel said the case of GP Harold Shipman, who was jailed in 2000 for murdering 15 patients, had "cast a long shadow" over events at the hospital.

The perception that Dr Barton might be a "lone wolf" operating alone "rapidly took root", the report said.
Police did not pursue a "wider investigation" into what was going on at the hospital and instead focused on the actions of Dr Barton. Hampshire Police said it would be taking "time to properly digest the significance of what has been revealed".
Chief Constable Olivia Pinkney said on Thursday: "It is already apparent from our early reading of the 370 pages that in its deliberations, the panel has had sight of information that has not previously been seen by Hampshire Constabulary.
"It is important that a process is put in place to ensure that all of the relevant agencies come together, to enable decisions about next steps to be made in a way that is well considered and transparent to all of the families."

Families demand 'rigour of criminal justice system'
Bridget Reeves, the granddaughter of 88-year-old Elsie Devine, said in a statement on behalf of the families: "This has been sinister, calculated and those implicated must now face the rigour of the criminal justice system.
"Accountability must take precedence here. These horrifying, shameful, unforgivable actions need to be disclosed in a criminal court for a jury to decide and only then can we put our loved ones to rest."

Whistleblowers still 'fired, gagged and blacklisted'
Health safety expert Professor Sir Brian Jarman, head of the Dr Foster Unit at Imperial College London, said the Gosport scandal could be repeated.
He said information on mortality rates produced by the unit was not properly assessed by health officials.
"There really is a desire not to know," he said, adding that whistleblowers were still "fired, gagged and blacklisted".
Asked on the Today programme if he would be surprised if events similar to Gosport were happening in other hospitals he said: "Not at all." He added: "I think it's likely."
Nurses concerns that went 'unheeded'
The Gosport Independent Panel found that hospital management, Hampshire Police, the Crown Prosecution Service, General Medical Council and Nursing and Midwifery Council "all failed to act in ways that would have better protected patients and relatives".
Its report also highlighted failings by healthcare organisations, local politicians and the coronial system.
The inquiry revealed "there was a disregard for human life and a culture of shortening lives of a large number of patients" at the Hampshire hospital.

The report added: "There was an institutionalised regime of prescribing and administering 'dangerous doses' of a hazardous combination of medication not clinically indicated or justified, with patients and relatives powerless in their relationship with professional staff."
Concerns were first raised by nurses in 1991 but these warnings went "unheeded".
When relatives later complained, from 1998, they were "consistently let down by those in authority, both individuals and institutions".

At a glance: What the Gosport report found
Here are the key findings of the Gosport Independent Panel:
A pattern of concerning opioid prescribing at Gosport War Memorial Hospital appears to have started in 1989 and ended in 2000. Nurses first raised concerns in 1991 but the warnings were "unheeded".
Evidence was found of opioid use "without appropriate clinical indication" in 456 patients.
Taking into account missing records, at least another 200 patients were "probably" also affected.
There was a "disregard for human life and a culture of shortening the lives of a large number of patients".
There was an "institutionalised regime" of prescribing and administering "dangerous doses" of drugs without medical justification.
Over a 12-year period, clinical assistant Dr Jane Barton, was responsible for prescribing.
Nurses had the responsibility to challenge prescribing, but continued to administer the drugs.
Consultants were not involved in treating patients, but were aware of how drugs were being prescribed and "did not intervene to stop the practice".
Patients and relatives were "powerless" in their relationship with professional staff.
When relatives complained about the safety of patients and appropriateness of their care they were "consistently let down" by individuals and authorities.
The senior management of the hospital, healthcare organisations, Hampshire Police, local politicians, the coronial system, the Crown Prosecution Service, the General Medical Council and
Te Nursing and Midwifery Council "all failed to act in ways that would have better protected patients and relatives".
Guilty of misconduct - but no charges brought
In 2010, the General Medical Council ruled that Dr Barton, who has since retired, was guilty of multiple instances of professional misconduct relating to 12 patients who died at the hospital.
After the GMC findings, the Crown Prosecution Service announced that there was insufficient evidence for a prosecution on charges of gross negligence manslaughter.
Several documents reviewed by the panel referred to the Shipman case. However the Rt Rev Jones said events at the Gosport War Memorial Hospital were distinct, because they showed a "failure of the institution".
Nurses on the ward were not responsible for the practice but did administer the drugs, including via syringe drivers, the panel said.

 Yahoo News
Yahoo News 
