What to do if you’re a Londoner worried about gonorrhoea? Test yourself, apparently | Nichi Hodgson
Like any thriving cosmopolis, London is a place of risk and reward. You’re never more than a hot breath away from someone throwing caution to the wind.
This happens with the things we shouldn’t be risking as much as with those we should. London has significantly higher rates of STI infection than the rest of the country, for instance, with more than 100,000 cases a year – with Chelsea being the seat of the most new infections.
But for the first time since the second world war, the sexual health of Londoners is on the line. Why? Because if you have gonorrhoea or syphilis or even potentially HIV, six major specialist clinics that would have been able to help have been shut. With an unprecedented strain put on the remaining services, self-testing kits to be distributed in 27 councils and accessed through a web portal were announced as the bandage to this wounded system. But due to reasons not given, they are unavailable until at least January – unless you shell out about £90 yourself.
Imagine if we were told penicillin for adults wouldn’t be available until the new year – there would be an outcry. But because it’s sexual health treatment, the story goes unreported, the outrage unvoiced, and the government effectively benefits from the stigma attached to seeking out sexual health services. Bad news is buried in cultural shame, and only a handful of campaigners are left with the capacity to talk about it.
That shame is the reason sexual health has long been treated as a “secondary” care issue, even when we know the ramifications of not making provision for it – everything from HIV infection – to infertility – are devastating. Since 2013, Londoners have relied on their local authorities to allocate funds to services that are delivered in conjunction with clinical commissioning groups and NHS England.
Each year, as the population grows, the demand for services increases. But as health budgets have been cut by the government, local authorities have found themselves having to turn patients in need away from clinics. Only a few months ago the World Health Organization warned against a pandemic of “super gonorrhea”, a strain so pernicious that it is resistant to all current antibiotics. There was no public health campaign, no free condom distribution, no increased testing and no advice on what to do if you thought you were infected, despite it posing a significant health threat to a city which had only just managed to stem the rising tide of regular gonorrhoea transmissions.
In the meantime, all other STIs are rising. Condoms are crucial but there are some that even condoms don’t cover. Take herpes. Symptoms can take months to come to the fore after transmission, during which time you could have passed the virus on. The only thing that truly protects your sexual health is regular testing – and someone to talk to you about the ramifications of certain sexual practices and to guide you if you find yourself infected.
The only thing that truly protects your sexual health is regular testing – and someone to talk to you if you're infected
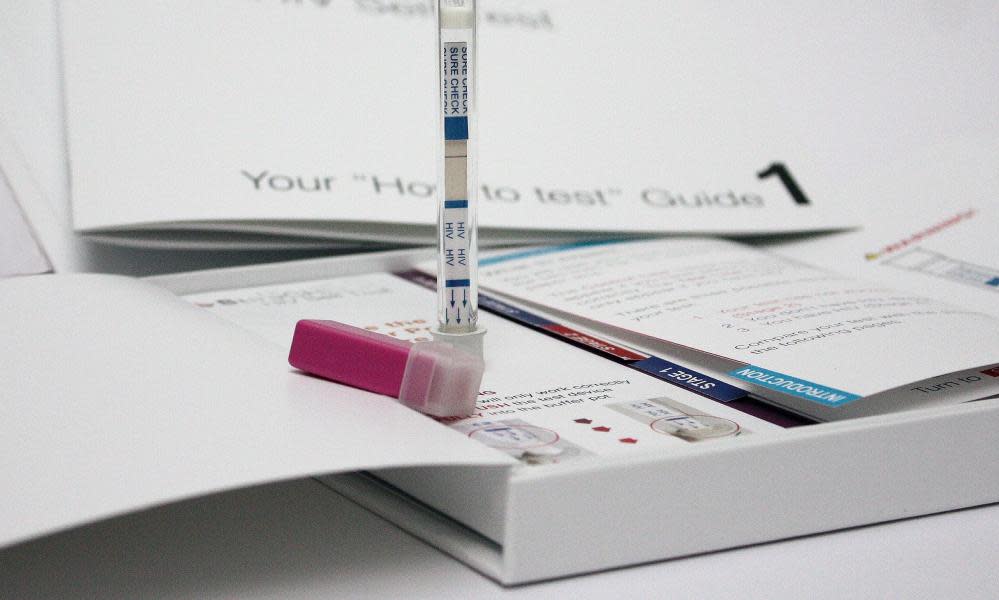
Yet the solution to London’s STI rates hasn’t been to mass-distribute condoms, properly fund sex education, campaign with notable celebrities who could help to normalise clinic trips, or even increase provision of clinical services. It has been to champion self-testing, (albeit with little to no advertising), encouraging people to order kits online of their own volition and to take the tests at home.
Self-testing might be convenient but convenience alone can’t overcome cultural embarrassment. For it to be successful, users need to be even more proactive and aware when it comes to dealing with their sexual health needs than the average clinic patient. Besides, as Dr Sarah Welsh, sexual health practitioner and founder of Hanx condoms, a disruptive brand trying to empower women to take charge of prophylactics, explains, “So many STIs do not have any signs or symptoms – it simply wouldn’t occur to many people to proactively access these self-testing kits”.
What’s more, self-testing can only generate part of the solution. “Meeting a health professional in person allows you to discuss other elements of sexual health,” continues Walsh. “It ensures examination, allowing you to pick up any other issues – including incidental findings of cancers, infections, and other potential unrelated health issues.” And if you need counselling or mental health support, you won’t find that neatly sealed in a package that pops through the letterbox.
If physicians know that self-testing can only be an effective part of treatment if run in tandem with existing services, it seems improbable that those responsible for London’s strategy don’t too. What’s more, London with its high number of sexual partners per capita has additional sexual health needs to the rest of the UK. One in four STI infections in the UK occurs in London, which includes more than half of the UK’s gonorrhoea infections, an alarming – and climbing – syphilis and chlamydia rate, while as many as one in seven gay or bisexual men live with HIV. And it’s not just young people indulging in chemsex, as the popular narrative would have it, who are responsible for new transmissions – HIV infections in the over-50s have actually increased at a faster rate.
Make no mistake: when it comes to London’s sexual health, the bodged handover from personal consultation to self-testing, couched in the language of “empowering” patients, is primarily a money-saving exercise. Yet a cursory look at the figures can tell you this is not the time to be cutting back on services. Arguably, we showed more commitment to public sexual health 100 years ago when we implemented the Defence of the Realm Act, which made it a criminal offence to infect a first world war soldier with venereal disease.
Put simply, we are neither practically nor culturally ready for DIY STI diagnosis. And the livelihood of the capital is at stake.
• Nichi Hodgson is a sex and relationship broadcaster

 Yahoo News
Yahoo News 
