STI warning as clinics close in London and self-testing is delayed
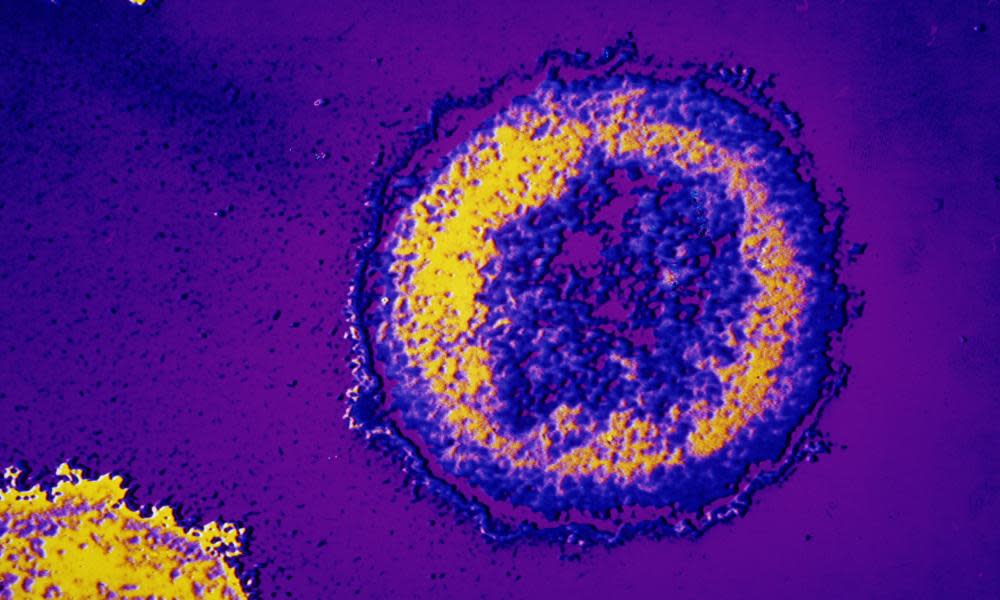
People are being denied care at overburdened sexual health clinics after a wave of closures and huge delays to a controversial new self-testing scheme for diseases such as herpes and syphilis, health experts are warning.
Six long-established sexual health clinics around London have shut in recent months as part of a planned switch from face-to-face consultations to online services.
Problems accessing services for sexually-transmitted infections (STI) are being compounded because the internet-based system, via which people can order a home-testing kit, is many months behind schedule.
“We are hearing about emerging evidence that shows patients are being turned away from sexual health services in London because of huge pressures clinics are facing,” said Dr Elizabeth Carlin, president of the British Association for Sexual Health and HIV (BASHH), which represents specialist doctors in the field.
The self-testing scheme was supposed to be rolled out across 27 of the capital’s 32 boroughs from 1 May. But it is still not functioning and will not start until January at the earliest.
Sexual health experts are warning that the clinic closures and unavailability of the kits could lead to “an explosive increase” in STI rates in London, which are already the highest in England.
“A lot of services are being dismantled and potentially that will have a big impact on the future of STI rates. The rates will go up substantially if we don’t get a handle on this,” said Dr Paul Lister, who until June helped run sexual health services in south-west London.
“The diagnosis of STIs will not be as efficient because people cannot access testing, so people who have untreated infections are more likely to have complications and potentially develop infertility. They are more likely to pass on infections to others as they will go undetected”, he added.
Levels of HIV infection could also start to rise again, Lister added. “Rates of HIV have gone down significantly in recent years. So if we reduce access to services, as is happening across London, we are doing that at our peril because history repeats itself and we see a direct link between access to services and rates of infection and the potential consequences of that.”
Kat Smithson, director of policy and campaigns at the National Aids Trust, said: “There seems to be a gap between the e-service being up and running and services it was supposed to support being closed. We are worried about the order things are happening in.
“From a patient perspective it changes your options and makes it harder to get an appointment, which seems to be what is happening.”
The restricted access threatens to undermine London’s success in encouraging gay and bisexual men to get tested, Smithson added. Men who have sex with men account for one in four STIs in the capital.
The 27 councils have given Preventx, a private diagnostics firm, the contract to provide the kit delivery service. They said that in future “the front door into services for most people will be web-based, with a single web address providing patients with information about sexual health, signposting to the most appropriate service for their needs and the ability to order self-sampling tests”. Councils were made responsible for funding many sexual health services, including STI testing as well as contraception, in 2013 in a massive shake-up of the NHS.
Councils acknowledged that “there may be fewer major centres for people with more complex sexual health needs” as a result of the clinic closures, more of which are due, but said “an online service will complement face to face clinic services”. The e-testing system is a key part of the London sexual health transformation programme, through which the councils are aiming to modernise sexual health care to cope with growing demand.
Some people who find that they cannot yet order a kit for free from Preventx are being offered a 10% discount on the usual £99.99 cost of a test for 10 common STIs, including chlamydia and gonorrhoea, from the company’s sister site test.me.
The sexual health clinics that have shut their doors include those at the Royal Free hospital in Hampstead and the Clare Simpson Clinic at Barnet hospital, both in north London, as well as two in south London run by Guy’s and St Thomas’ NHS Trust.
Sexual health experts claim the changes in London have been forced on councils by ministers cutting the amount of money they give them for public health work. Public Health England warned in a recent report that local councils could not maintain their current level of sexual health services as a direct result of those cuts.
A spokesperson for London Sexual Health Transformation Programme said: “The e-service and self-sampling kits offer a new way for people to access services that makes the best use of new technology, recognises the changing way people get their information and health care and frees up face to face clinic appointments for those with greater need.”

 Yahoo News
Yahoo News 
