Why is it that while Covid-19 cases are rising, deaths continue to fall?
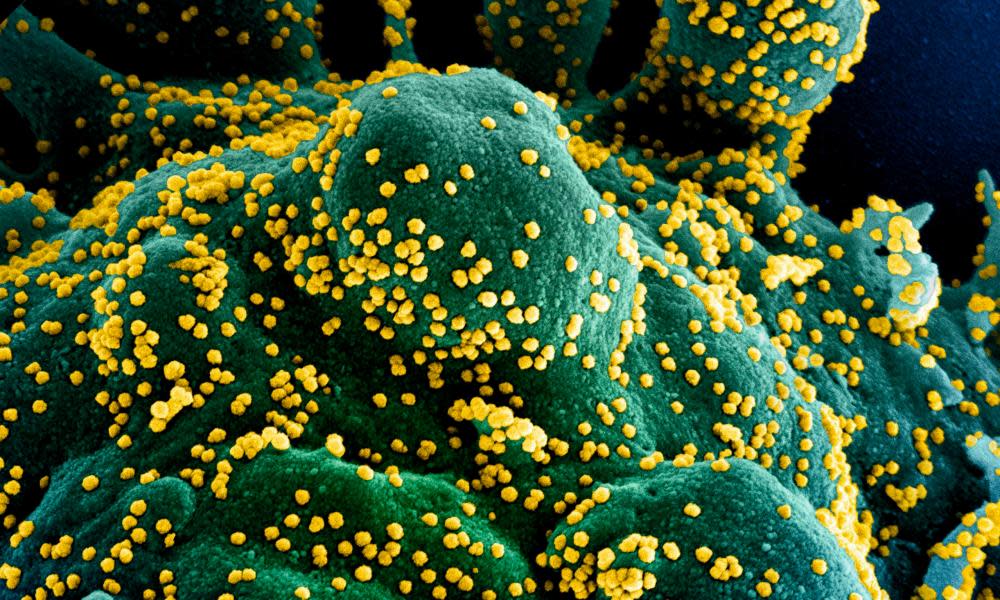
The government’s Covid-19 dashboard shows cases have risen steadily from their lowest point on 1 July when the rolling seven-day average was down to 574. By 30 August it had more than doubled, to 1,402 a day. Yet the death rate has declined steadily over the same period: from a rolling average of 37.4 per day to 4.6 per day. No one is sure why. But here are some explanations researchers are examining:
Are new patients less likely to die because they are younger?
More than two-thirds of new cases in the last week of August were people under 40, according to Public Health England, a figure which is likely to be linked to looser rules on socialising. At the peak of the pandemic, only 28% of cases were younger than 40.
The risk of dying from Covid-19 doubles at roughly every six years of age, according to professor David Spiegelhalter, so the 2,042 people in their 20s who caught Covid-19 in the last week of August were unlikely to need treatment.
Are vulnerable people still shielding?
Far fewer people over 70 tested positive for Covid-19, according to the PHE data – 374 in the last week of August, compared with 10,770 in the first week of April.
People in this age group are likely to remain at risk of becoming seriously ill if they become infected.
However, most of them are taking care not to, or are being protected, according to Dr Veena Raleigh, a senior fellow at the King’s Fund, an independent charitable healthcare body.
Do hospitals have better treatments?
Researchers at Oxford have published analysis showing that people with the virus in June were four times less likely to die in hospital than in April.
There are several factors playing a part: doctors switched from ventilators, which pump oxygen directly into the lungs with a tube, to using non-invasive devices such as CPAP. Infection control improved as hospitals created Covid-19 wards, and hospitals are quieter, reducing pressure on clinicians. The steroids dexamethasone and hydrocortisone both also improve chances of recovery by calming the body’s immune response.
Does more testing mean more mild cases are discovered?
In March and April, testing was limited almost entirely to hospital patients and staff. The lacuna of community transmission has slowly been filled by an increase in “Pillar Two” drive-through and walk-in testing sites, and nearly 90% of new cases are identified this way, PHE figures show.
Prof Carl Heneghan at Oxford’s Centre for Evidence-Based Medicine also says tests may be too sensitive and detect small amounts of virus in those who recovered weeks before.
Do social distancing measures mean viral loads are lower?
There may be a link between social distancing and viral load – the amount of virus present in a body. Some research shows that wearing masks and keeping away from other people reduces the amount of virus they are exposed to. And a Lancet study found that the amount of virus present when a patient was tested did predict how likely patients were to die.
Has vitamin D from sunshine helped?
Some researchers have suggested a link between vitamin D deficiency and Covid-19 death rates, and people have advocated the vitamin as a treatment for respiratory diseases for nearly a century. A study by the University of Chicago last week showed people with vitamin D deficiency were almost twice as likely to test positive for the virus as those with healthy levels. However, transmission rates soared during summer in the US, so any broader health impact seems limited.
Are there fewer vulnerable people left?
So far at least 21,775 of those who died in the UK were care home residents. Yet the total care home population alone is 330,000 and another 350,000 receive care at home. So there are still large numbers at a higher risk of serious illness.
Are we starting to see herd immunity?
Antibody testing studies have estimated that about 13% to 17% of Londoners have had the virus, a much higher figure than seen elsewhere in the UK, but much lower than the 70% that is assumed as the lowest level to be needed to achieve herd immunity. Immunity for other respiratory coronaviruses such as the common cold can last for months but then fades, so there is no guarantee that those who have been infected can brush off Covid-19 for ever. Herd immunity ought to lead to fewer people becoming infected, rather than less serious effects of infection.
Is Covid-19 getting weaker?
Geneticists have discovered that there is some evidence Covid-19 is evolving, but so far there does not seem to be any solid evidence that it is becoming less dangerous – or, thankfully, more deadly either.

 Yahoo News
Yahoo News 
