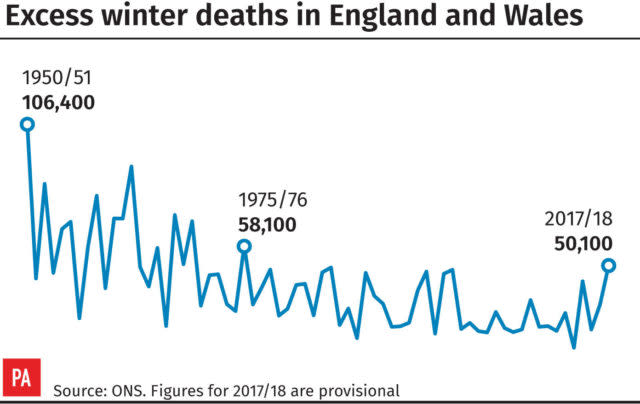
Excess winter deaths increase to highest level for more than 40 years
There were an estimated 50,100 excess winter deaths in England and Wales in 2017/18 – the highest recorded since winter 1975/76, figures show.
The increase is thought to be down to the flu, the effectiveness of the flu vaccine and the particularly cold weather seen last winter.
The data, from the Office for National Statistics (ONS), also shows that more than a third (34.7%) of the deaths were caused by respiratory diseases.
Excess winter mortality continued to be highest among females and people aged 85 and over, while it doubled among males aged 0-64 between the winter of 2016/17 and 2017/18.
The number of daily deaths exceeded the five-year average for all dates except March 25.
Nick Stripe, head of health analysis and life events at the ONS, said: “The number of excess winter deaths in England and Wales in 201718 was the highest recorded since the winter of 1975/76.
“However, peaks like these are not unusual – we have seen more than eight peaks during the last 40 years.
“It is likely that last winter’s increase was due to the predominant strain of flu, the effectiveness of the influenza vaccine and below-average winter temperatures.”
The number of excess winter deaths was significantly higher across all regions, but it was highest in Wales https://t.co/U0npTR3JPq pic.twitter.com/bsW08M4kPL
— ONS (@ONS) November 30, 2018
The ONS said the increases could be explained partly by temperature, as colder weather was observed in December, February and March compared with the five-year average.
Specifically, central England daily temperatures show there was a particularly cold period between February 22 and March 3, which could account for the second peak in daily deaths.
The peak in January could also be a result of flu, which saw increased levels in the first weeks of January, reaching a peak in week three.
Statisticians said the high number of deaths among the over-85 age group may be due to the circulation of influenza A and influenza B, which predominantly affected older adults.
The number of excess winter deaths observed in 2017/18 was higher than all years since the 1975/76 winter period, when there were 58,100 deaths.
However, the increase was similar to peaks observed in previous years such as 2014/15, 1999/2000 and 1998/99.
Compared with recent years, excess winter deaths observed in 2017/18 were 45.1% higher than the 2016/17 winter and more than double those seen in 2015/16.
The most recent peak was seen in 2014/15, although winter 2017/18 exceeded this by around 6,000 deaths.
The figures also showed that excess winter mortality in 2017 to 2018 significantly increased from 2016 to 2017 in all English regions and Wales, and those affected the most were females and people aged 85 and over.
Commenting on the findings, Age UK’s charity director, Caroline Abrahams, said: “A toxic cocktail of poor housing, high energy prices and ill-health can make winter a dangerous time for many older people, and tragically it is the oldest and those who are the most vulnerable who particularly suffer the consequences.”
Dr Veena Raleigh, senior fellow at the King’s Fund think-tank, said: “These figures show the grim reality that many older people died in winter 2017/18 after a severe flu outbreak.
“This follows some other recent winters when seasonal deaths have been high. With an ageing population, the worry is that this could be the start of a trend of periodically high winter deaths.
“National agencies have so far been slow to respond to these disturbing recent trends. Public Health England has been commissioned to investigate the slowdown in life expectancy and it is imperative that their findings are acted upon.”
Ian Hudspeth, chairman of the Local Government Association’s community well-being board, said the figures were “hugely concerning”.
“There are too many avoidable deaths each winter in England, primarily due to heart and lung conditions from cold temperatures rather than hypothermia,” he added.
“Reducing excess winter illness and death is not something that can be tackled in the winter alone nor something that the NHS alone can fix.
“With the imminent publication of the NHS long-term plan and the Government’s Green Paper on the future of social care, and the Secretary of State’s focus on prevention, the Government has an important opportunity to take a truly system-wide approach to supporting people’s well-being.”

 Yahoo News
Yahoo News 
