Long Covid sufferers 'face psychiatric problems as well as pain and fatigue'


Many sufferers of “long Covid” can endure psychiatric problems, as well as pain and fatigue, the National Institute of Health and Care Excellence has warned.
The body, which is drawing up guidelines on how to treat the condition, says it should be considered in anyone who appears to have symptoms 12 weeks after the first ones appeared, when there is no alternative explanation.
Experts said that a “sizeable minority” of sufferers could continue to suffer symptoms after three months, regardless of how severe their original infection was.
New documents, setting out the scope of the guidance, are being drawn up with the Royal College of GPs. They say the diagnosis should be considered when symptoms persist, after an acute episode of Covid, regardless of whether the patient was tested.
While symptoms often overlap, and cluster, just one symptom - such as persisting fever, pain or psychiatric problems - could be enough to consider a diagnosis, the organisations say.
The guidance on how to treat the condition will be published by the end of the year.
The guideline scope published on Friday, October 30, defines post-Covid syndrome (also known as Long Covid) as “signs and symptoms that develop during or following an infection consistent with Covid-19 which continue for more than 12 weeks and are not explained by an alternative diagnosis”.
It says the condition usually presents with clusters of symptoms, often overlapping, which may change over time and can affect any system within the body.
Nice said that “many people with post-Covid syndrome can also experience generalised pain, fatigue, persisting high temperature and psychiatric problems”.
Paul Chrisp, the director of the Centre for Guidelines at Nice, said: “Recovery from any infectious illness can take time and although most people with Covid-19 will recover completely within a few weeks from the onset of symptoms, we know that a sizeable minority will continue to have symptoms for 12 weeks or more afterwards, regardless of how ill they were initially or whether they were hospitalised.
“This is a new condition and there is still a lot we don’t know about it. Our aim is that the post-Covid syndrome guideline will begin by setting best practice standards of care based on the current evidence but, as our understanding of the condition grows, be adaptable and responsive to new evidence as it emerges.”
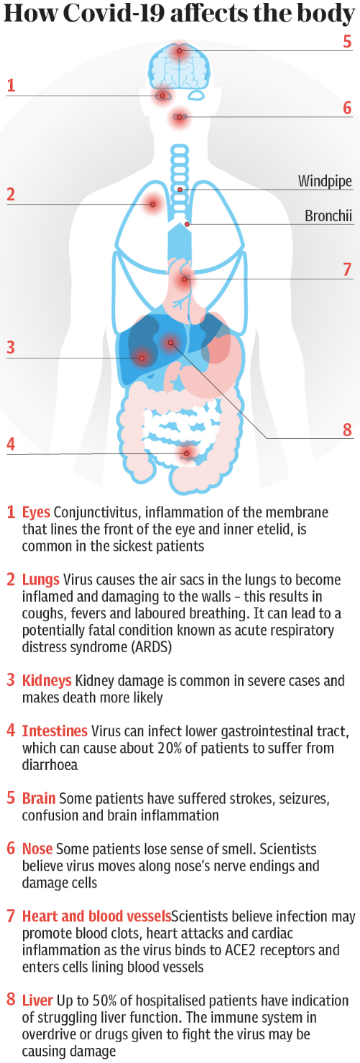
The guidance says: “Signs and symptoms may arise from any system in the body, often overlap, and may change over time. This includes but is not limited to the cardiovascular, respiratory, gastrointestinal, neurological, musculoskeletal, metabolic, renal, dermatological, otolaryngological, haematological and autonomic systems, in addition to psychiatric problems, generalised pain, fatigue and persisting fever.”
Those with “one or more ongoing symptoms” will be included in the definition.
The guidance is being drawn up in conjunction with the Scottish Intercollegiate Guidelines Network (Sign) .
The scope outlines what areas the guideline will cover. These will include what symptoms or signs should prompt a referral for specialist assessment or management, what pharmacological and non-pharmacological interventions improve physical or mental health symptoms following acute Covid-19, and how best to deliver post-Covid syndrome recovery and rehabilitation services.
Safia Qureshi, the director of evidence for Healthcare Improvement Scotland, of which Sign is a part, said: “We understand that Long Covid is creating great distress and uncertainty for those affected, and that the NHS requires the best available advice to support people effectively, even as we continue to seek to understand it.
"The scope report is a first and vital stage in the production of a guideline which aims to identify symptoms and outline treatment options. We’re delighted to work with Nice and the RCGP on this important piece of work.”
Prof Martin Marshall, Chair of the Royal College of GPs, said: “Before we can effectively diagnose, treat and manage a condition, we need to know what we’re dealing with, so it’s encouraging to be making such rapid progress in this regard as we work with NICE and SIGN to develop this important guidance.
"The prolonged health effects that some patients experience after contracting Covid-19 can have a terrible impact on their lives – and as GPs, we want to do what we can to help them.
“Now that we are clear about its scope, we can move forward in developing guidance, based on the latest evidence, to support GPs to deliver the most appropriate care and support to patients suffering with the long-term effects of Covid-19 in the community.
"This guidance will need to evolve as our understanding of the condition grows through clinical experience and robust research”.

 Yahoo News
Yahoo News 
