Rising maternal deaths deserve attention in N.B. and other provinces, say obstetricians
The former head of perinatal care in New Brunswick and current president of the Society of Obstetricians and Gynaecologists of Canada is calling on provinces, including New Brunswick, to do a better job of tracking maternal mortality.
"I can tell you that we're not good at it — just like many other provinces," said Dr. Lynn Murphy-Kaulbeck, who practised in the province for more than 18 years and now teaches at Dalhousie University's medical school in Nova Scotia.
Better information is the first step to reversing an upward trend in maternal mortality, she said.
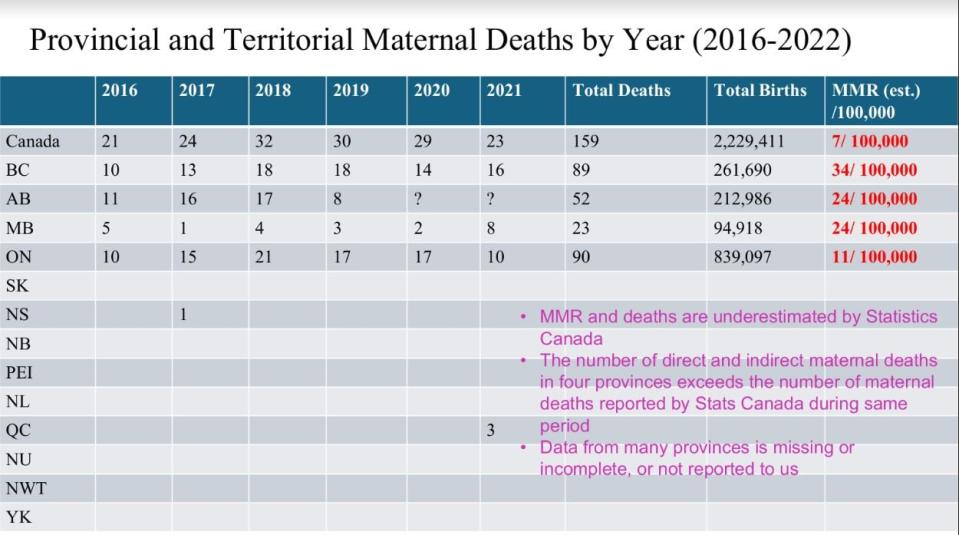
According to the World Health Organization, Canada's maternal mortality ratio has increased from about nine to 11 deaths per 100,000 births over the last two decades.
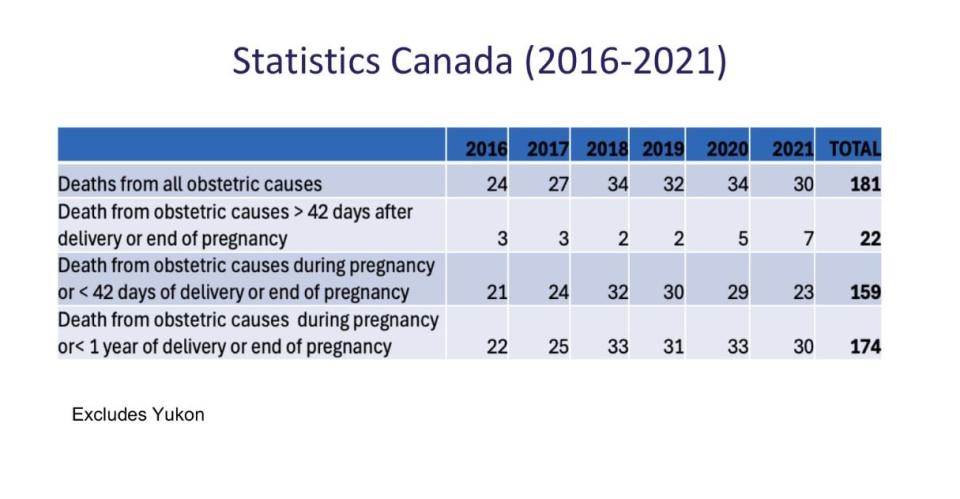
The true rate is probably even higher than that, said Murphy-Kaulbeck.
That's because most of the federal data is from vital statistics and hospital discharge databases, both of which underestimate maternal deaths, she said.
For example, if a woman dies sometime in the postpartum period, which is 42 days after delivery, and there's no mention on the death certificate that she'd been pregnant, "it would never be flagged as a maternal death."
Maternity can be an indirect cause of death in cases of postpartum depression leading to suicide, intimate partner violence or addictions, said Murphy-Kaulbeck.
"We don't capture those well," she said.
Murphy-Kaulbeck is urging the provinces and the federal government to collaborate on a data collection system that identifies all deaths, near deaths, and severe illnesses related to pregnancy.
She said they need to sit down together and decide what needs to be collected, how it's collected and how the information will be used to look for root causes, assess contributing factors such as addiction, mental health and socioeconomic status and target preventative measures.
The United Kingdom has a good system for maternal death prevention, said Murphy-Kaulbeck.
In that country, every maternal death is reviewed by confidential inquiry and their numbers are trending down, she said.
In Canada, Ontario is one of a few provinces that tracks maternal mortality.
According to the Ontario coroner's service, it has a committee made up of doctors, midwives and nurses that reviews all maternal deaths during pregnancy, delivery, the postpartum period and sometimes even later if there are concerns it was related to the pregnancy. It also reviews stillbirths and perinatal deaths if issues have been flagged.
The committee's most recently published annual report is from 2020, when 23 cases were reviewed and 39 recommendations were made.
For example, one case involved a 24-year-old previously healthy woman who died of sepsis from a Group A streptococcus infection three days after giving birth.
A recommendation of the committee was to encourage hospitals to use a risk assessment tool called the modified early obstetric warning system or MEOWS.
In another case, a 40-year-old pregnant woman died of pulmonary embolus a few days after seeking medical attention for swelling in her leg.
The committee issued a reminder to obstetricians of the signs and urgency of deep vein thrombosis and the need for thorough documentation of what takes place during virtual appointments.
A third case was a 39-year-old woman who had recently arrived from Bangladesh and died of postpartum hemorrhage. It had been previously noted in her file that she was at high risk of postpartum bleeding, but it wasn't clear whether that information had been conveyed and appointments had been missed.
The committee encouraged caregivers to use translation services or community resources when language or cultural factors could impact the patient's ability to comprehend care plans and make informed choices.
Toolkit in the works for provinces to use
The national obstetrician group is working in conjunction with Ontario and the other provinces currently collecting maternal mortality data on a toolkit that other provinces can implement, said Murphy-Kaulbeck.
Getting the required data is cumbersome, she said, because the federal government is responsible for collecting national data, but the provinces are responsible for delivering health care and deciding what data to collect.
Data sharing is also a challenge when it comes to tracking other things including stillbirths, she said.
"New Brunswick, like many other provinces, has work to do. But I have every confidence they'll do it," said Murphy-Kaulbeck.
"This isn't going to happen overnight. But I think we have momentum."
CBC News asked the New Brunswick Health Department what it knows about maternal death numbers in the province and whether any changes to improve tracking or prevention are in the works. No response was available at publication time.

 Yahoo News
Yahoo News 
